Social Media Posts
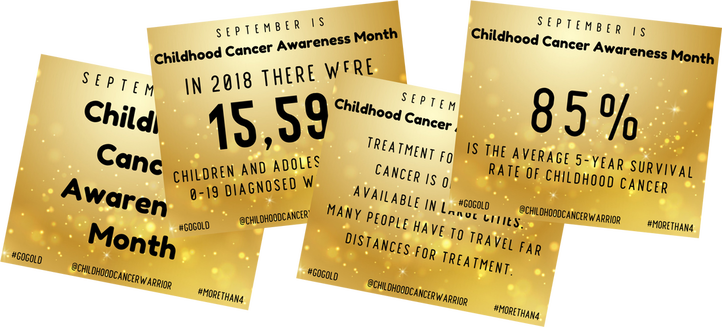
These facts can be posted one a day on Instagram or Facebook stories. They can also be posted as a post on Facebook. Click the link to download the files to help spread awareness during the month of September and every other month!
All About Cancer - Daily Facts (Day 1-30)
Childhood Cancer Awareness Month Daily Facts (Day 1-30 with 3 bonus facts)
Will You Go Gold With Me? Posts
Cancer Facts and Information to Post*
*keep checking to see what is new - new post will be added frequently
Sparkle Gold - September Posts
Click on each drop-down box to copy and paste the text if you want to post it each day on your social media platforms. There is also a graphic that goes along with the text. You can copy and paste the text to your social media platforms and if you click the box under the photo, it will take you to the folder to download and save the graphic.
Please make sure that you tag us in your posts! We want to see how far our reach is.
Use hashtags: #childhoodcancerwarriors #CCW #CCW23
Please make sure that you tag us in your posts! We want to see how far our reach is.
Use hashtags: #childhoodcancerwarriors #CCW #CCW23
Day 1
Day 1 of #childhoodcancerawareness month and I want to show my Facebook world just how UNRARE childhood cancer is.
If your child is a fighter, survivor, or an angel can you please comment below. I want to put names and faces so people can see how devastating childhood cancer really is and how it is not rare at all!
Did you know that Illinois is ranked #24 out of 50 in the country of overall incident rates of childhood cancer!
17th- Leukemia overall incidence rates of childhood cancer
23rd- Lymphoma overall incident rates of childhood cancer
33rd- Brain & CNS overall incident rates of childhood cancer
20th- Soft Tissue Sarcoma overall incident rates of childhood cancer
15th- Other Epithelial Neoplasms overall incident rates of childhood cancer
We need to do better for our kids!
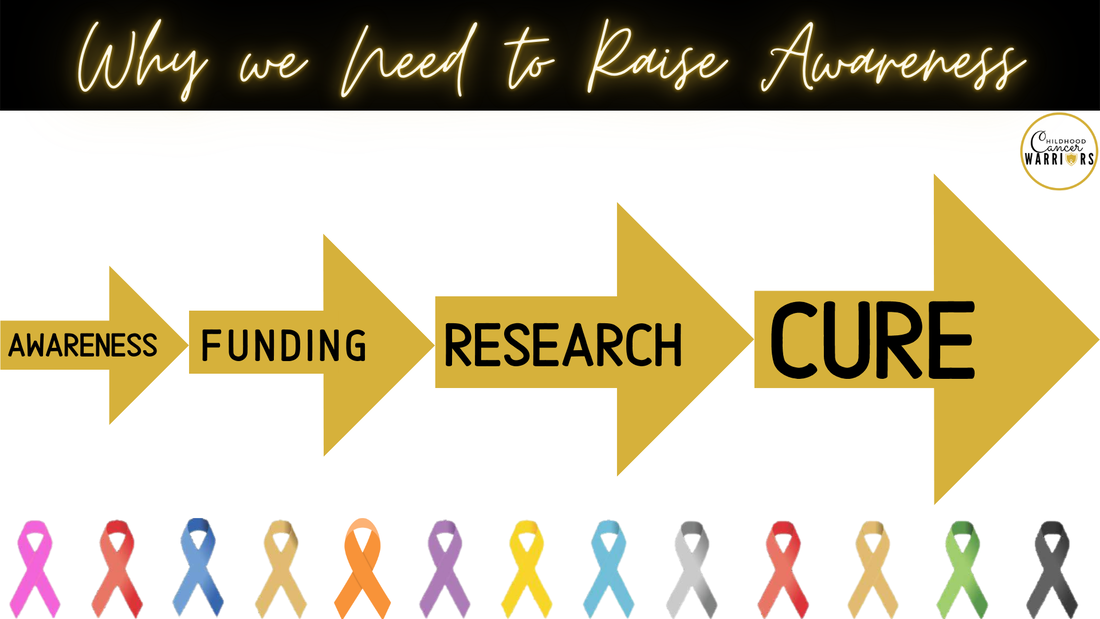
Awareness=Funding=Research=A Cure
#journeyofaleukemiawarrior #ccam2023 #CCAM #morethan4 #childhoodcancerwarriors #childhoodcancerawareness
If your child is a fighter, survivor, or an angel can you please comment below. I want to put names and faces so people can see how devastating childhood cancer really is and how it is not rare at all!
Did you know that Illinois is ranked #24 out of 50 in the country of overall incident rates of childhood cancer!
17th- Leukemia overall incidence rates of childhood cancer
23rd- Lymphoma overall incident rates of childhood cancer
33rd- Brain & CNS overall incident rates of childhood cancer
20th- Soft Tissue Sarcoma overall incident rates of childhood cancer
15th- Other Epithelial Neoplasms overall incident rates of childhood cancer
We need to do better for our kids!
Awareness=Funding=Research=A Cure
#journeyofaleukemiawarrior #ccam2023 #CCAM #morethan4 #childhoodcancerwarriors #childhoodcancerawareness
Day 2
Day 2 The day before diagnosis, I wasn't a cancer mom either...
I am wearing a pair of shoes. They are ugly shoes. Uncomfortable shoes. I hate my shoes. Each day I wear them, and each day I wish I had another pair. Some days my shoes hurt so bad that I do not think I can take another step.
Yet, I continue to wear them. I get funny looks wearing these shoes. They are looks of sympathy. I can tell in others eyes that they are glad they are my shoes and not theirs. They never talk about my shoes.
To learn how awful my shoes are might make them uncomfortable. To truly understand these shoes you must walk in them. But, once you put them on, you can never take them off. I now realize that I am not the only one who wears these shoes. There are many pairs in this world.
Some people are like me and ache daily as they try and walk in them. Some have learned how to walk in them so they don’t hurt quite as much. Some have worn the shoes so long that days will go by before they think about how much they hurt.
No one deserves to wear these shoes. Yet, because of these shoes I am a stronger person. These shoes have given me the strength to face anything. They have made me who I am. I will forever walk in the shoes of a person who had a child with Cancer.
-Author Unknown
I am wearing a pair of shoes. They are ugly shoes. Uncomfortable shoes. I hate my shoes. Each day I wear them, and each day I wish I had another pair. Some days my shoes hurt so bad that I do not think I can take another step.
Yet, I continue to wear them. I get funny looks wearing these shoes. They are looks of sympathy. I can tell in others eyes that they are glad they are my shoes and not theirs. They never talk about my shoes.
To learn how awful my shoes are might make them uncomfortable. To truly understand these shoes you must walk in them. But, once you put them on, you can never take them off. I now realize that I am not the only one who wears these shoes. There are many pairs in this world.
Some people are like me and ache daily as they try and walk in them. Some have learned how to walk in them so they don’t hurt quite as much. Some have worn the shoes so long that days will go by before they think about how much they hurt.
No one deserves to wear these shoes. Yet, because of these shoes I am a stronger person. These shoes have given me the strength to face anything. They have made me who I am. I will forever walk in the shoes of a person who had a child with Cancer.
-Author Unknown
Day 3
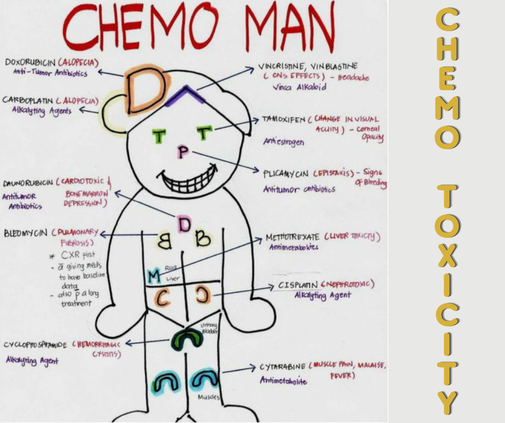
Day 3 - Pediatric Cancer Drugs
Imagine for a second that you’re told your child has cancer. Surely the treatments are cutting edge and curative, right?
This is 2021 after all.
You research the chemo drugs that your child will be receiving and you’re shocked to find that they’re older than your child’s grandparents.
How can this be?
We have self driving cars, a rover on Mars, virtual reality, and smart phones but haven’t found less toxic and more effective treatments for childhood cancer?
September is Childhood Awareness Month - so let’s raise some awareness!
Let’s make GOLD September as popular as PINK October!
#childhoodcancerawareness #gogoldforchildhoodcancer #gogoldinseptember #morethan4 #duckprints #ccam2021 #childhoodcancerwarriors #journeyofaleukemiawarrior
Imagine for a second that you’re told your child has cancer. Surely the treatments are cutting edge and curative, right?
This is 2021 after all.
You research the chemo drugs that your child will be receiving and you’re shocked to find that they’re older than your child’s grandparents.
How can this be?
We have self driving cars, a rover on Mars, virtual reality, and smart phones but haven’t found less toxic and more effective treatments for childhood cancer?
September is Childhood Awareness Month - so let’s raise some awareness!
Let’s make GOLD September as popular as PINK October!
#childhoodcancerawareness #gogoldforchildhoodcancer #gogoldinseptember #morethan4 #duckprints #ccam2021 #childhoodcancerwarriors #journeyofaleukemiawarrior
Day 4
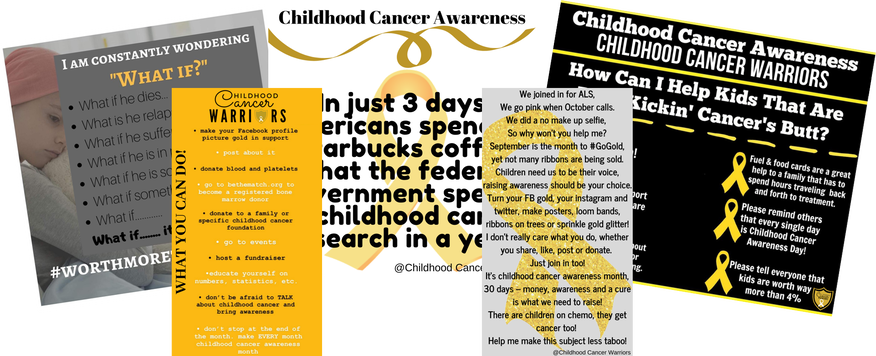
Day 4: What does #childhoodcancer Need?
Here is how you can help kids who are battling cancer!
#morethan4 #ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #gogoldforchildhoodcancer #gogold #childhoodcancerwarrior #GoGoldInSeptember
Childhood Cancer Warriors Journey of a Leukemia Warrior
Here is how you can help kids who are battling cancer!
#morethan4 #ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #gogoldforchildhoodcancer #gogold #childhoodcancerwarrior #GoGoldInSeptember
Childhood Cancer Warriors Journey of a Leukemia Warrior
Day 5
Day 5: Masks
As the pandemic hit, no one was more prepared to wear a mask all the time like a cancer kid and their families. They have been wearing a mask since their child started the fight of their life. There was no issue, it was just something they knew they had to do to stay healthy and safe.
As the global pandemic grew, we were asked to wear face masks for the protection and care of others and the greater good. Although masks are no longer mandated in many areas, it is still mindful to be aware of those around you, those who are at risk of covid and unable to be vaccinated for many reasons.
However uncomfortable masks are it will never match what children receiving radiation to certain parts of their body have to endure and the masks that they have to wear for hours and weeks at a time. The masks are even bolted to the table so they can no move.
Watch this video of the "masks" cancer kids have to wear and then I hope you will think twice about complaining that you or your child has to wear a mask in public places and schools.
I think we all know which mask we would rather have to wear.
We have a choice, let's carry on making the right one.
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #duckprints #gogoldforchildhoodcancer
As the pandemic hit, no one was more prepared to wear a mask all the time like a cancer kid and their families. They have been wearing a mask since their child started the fight of their life. There was no issue, it was just something they knew they had to do to stay healthy and safe.
As the global pandemic grew, we were asked to wear face masks for the protection and care of others and the greater good. Although masks are no longer mandated in many areas, it is still mindful to be aware of those around you, those who are at risk of covid and unable to be vaccinated for many reasons.
However uncomfortable masks are it will never match what children receiving radiation to certain parts of their body have to endure and the masks that they have to wear for hours and weeks at a time. The masks are even bolted to the table so they can no move.
Watch this video of the "masks" cancer kids have to wear and then I hope you will think twice about complaining that you or your child has to wear a mask in public places and schools.
I think we all know which mask we would rather have to wear.
We have a choice, let's carry on making the right one.
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #duckprints #gogoldforchildhoodcancer
Day 6
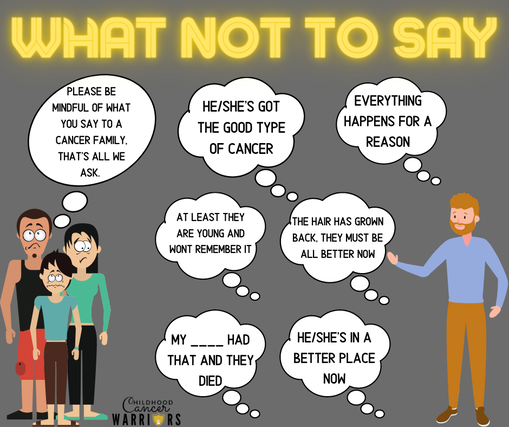
Day 6: What not to say to a cancer family
When a child, teen or young adult is diagnosed with cancer, people around them often struggle with what to say. We all recognize how this can be very difficult, however, being mindful about what is said can have a huge impact on the children and their parents. The wrong words or thoughtless comment can have a devastating and demoralizing effect on these families.
These are just some of the few that we have heard...they are so many more comments that people have said.
Here are six key pieces of advice I want to share when it comes to supporting families going through childhood cancer.
1. Don’t just ask “What can I do for you?”, Do Something!
2. Remember the siblings.
3. Even when remission is reached or chemo is finished, the fight is not over. Constantly check in on the family.
4. There is not a different or special treatment for pediatric cancer patients.
5. You may see a child with cancer looking “normal” with a full head of hair, laughing, playing, and smiling. That child is still sick. It’s a long road.
6. Pediatric/Childhood Cancer research is SEVERELY underfunded!
http://www.journeyofaleukemiawarrior.com/.../real-talk-6...
#makeseptembergold #childhoodcancer #childhoodcancerawareness #childhoodcancerawarenessmonth #whatnottosay #bemindful #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #duckprints #gogold #ccam2022
When a child, teen or young adult is diagnosed with cancer, people around them often struggle with what to say. We all recognize how this can be very difficult, however, being mindful about what is said can have a huge impact on the children and their parents. The wrong words or thoughtless comment can have a devastating and demoralizing effect on these families.
These are just some of the few that we have heard...they are so many more comments that people have said.
Here are six key pieces of advice I want to share when it comes to supporting families going through childhood cancer.
1. Don’t just ask “What can I do for you?”, Do Something!
2. Remember the siblings.
3. Even when remission is reached or chemo is finished, the fight is not over. Constantly check in on the family.
4. There is not a different or special treatment for pediatric cancer patients.
5. You may see a child with cancer looking “normal” with a full head of hair, laughing, playing, and smiling. That child is still sick. It’s a long road.
6. Pediatric/Childhood Cancer research is SEVERELY underfunded!
http://www.journeyofaleukemiawarrior.com/.../real-talk-6...
#makeseptembergold #childhoodcancer #childhoodcancerawareness #childhoodcancerawarenessmonth #whatnottosay #bemindful #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #duckprints #gogold #ccam2022
Day 7
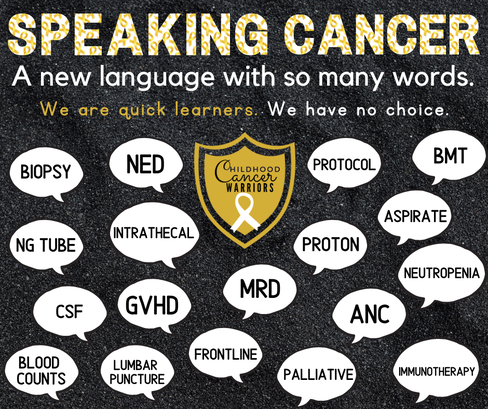
Day 7: Speaking Cancer
For most parents, few things are as frightening as hearing from the doctor that your child has cancer. Parents are dealing with their own fears and confusion at this time. Yet, they must also face the task of new faces, new places and a world of a completely different and strange language.
Parents are thrown in to this new world with out anyone to teach or help navigate these new and strange waters. Its either sink or swim. There is no time to study, its like you have slept all semester long in class and now you are at your final and have to know all of these unfamiliar terms.
"Speaking Cancer" is hard, understanding all the medical words and abbreviations and having to know what they mean on the spot to make critical decisions for our children is tough! The learning curve is huge and extremely steep but we do it. We learn these new words, we use them without thought and we engage in conversations with medical professionals using words that we didn't even know existed.
We know the names of blood cells, drugs, disease names, stages of the journey, drug interactions, procedures, and so on.
Parents of children with a cancer diagnosis are quick learners, we have no choice. We are our children's advocates and we will stop at nothing in our understanding of our children's journey.
Cancer moms joke that once they enter into a cancer journey, they should be given a framed and matted "honoree" medical diploma!
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogoldforchildhoodcancer #leukemiawarrior #lukasstrong #warriorlukas #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia
For most parents, few things are as frightening as hearing from the doctor that your child has cancer. Parents are dealing with their own fears and confusion at this time. Yet, they must also face the task of new faces, new places and a world of a completely different and strange language.
Parents are thrown in to this new world with out anyone to teach or help navigate these new and strange waters. Its either sink or swim. There is no time to study, its like you have slept all semester long in class and now you are at your final and have to know all of these unfamiliar terms.
"Speaking Cancer" is hard, understanding all the medical words and abbreviations and having to know what they mean on the spot to make critical decisions for our children is tough! The learning curve is huge and extremely steep but we do it. We learn these new words, we use them without thought and we engage in conversations with medical professionals using words that we didn't even know existed.
We know the names of blood cells, drugs, disease names, stages of the journey, drug interactions, procedures, and so on.
Parents of children with a cancer diagnosis are quick learners, we have no choice. We are our children's advocates and we will stop at nothing in our understanding of our children's journey.
Cancer moms joke that once they enter into a cancer journey, they should be given a framed and matted "honoree" medical diploma!
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogoldforchildhoodcancer #leukemiawarrior #lukasstrong #warriorlukas #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia
Day 8
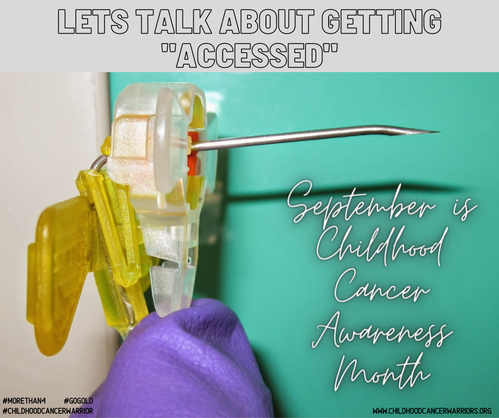
Day 8: Getting Accessed!
Maybe you have heard a cancer patient or family say that phrase before, but do you really know what "getting accessed" means? A Huber needle is a specially designed hollow needle used with a chemotherapy port (port-a-cath). The needle has a long, beveled tip that can go through your skin as well as the silicone septum of your implanted port's reservoir. Lukas' needle is a 20 or 21 gauge needle which is about 1 inch long.
This is how our children are accessed each time they go to clinic to receive treatments or chemotherapy. This needle is forced through their chest into their port-a-cath (more about this tomorrow), the devise that delivers the chemotherapy into the heart and bloodstream.
For many children, this is the hardest part. They fear getting accessed more than the treatments themselves. They look into your eyes, crying and screaming begging you to make it stop. All you can do is hold down your child, kiss their little foreheads, tell them that they are so brave and it will be over soon with a smile on your face. But inside you are falling apart! As parents, we can not stop this, as it is necessary to deliver the lifesaving drugs to our children.
This is childhood cancer.......
#journeyofaleukemiawarrior ##gogoldforchildhoodcancer #childhoodcancerawareness #cancermom #childhoodcancerwarrior #pediatriccancerawareness #morethan4 #septemberischildhoodcancerawarenessmonth #gogold #BeBoldGoGold #pediatriccancer #ccam #childhoodcancerwarriors
Maybe you have heard a cancer patient or family say that phrase before, but do you really know what "getting accessed" means? A Huber needle is a specially designed hollow needle used with a chemotherapy port (port-a-cath). The needle has a long, beveled tip that can go through your skin as well as the silicone septum of your implanted port's reservoir. Lukas' needle is a 20 or 21 gauge needle which is about 1 inch long.
This is how our children are accessed each time they go to clinic to receive treatments or chemotherapy. This needle is forced through their chest into their port-a-cath (more about this tomorrow), the devise that delivers the chemotherapy into the heart and bloodstream.
For many children, this is the hardest part. They fear getting accessed more than the treatments themselves. They look into your eyes, crying and screaming begging you to make it stop. All you can do is hold down your child, kiss their little foreheads, tell them that they are so brave and it will be over soon with a smile on your face. But inside you are falling apart! As parents, we can not stop this, as it is necessary to deliver the lifesaving drugs to our children.
This is childhood cancer.......
#journeyofaleukemiawarrior ##gogoldforchildhoodcancer #childhoodcancerawareness #cancermom #childhoodcancerwarrior #pediatriccancerawareness #morethan4 #septemberischildhoodcancerawarenessmonth #gogold #BeBoldGoGold #pediatriccancer #ccam #childhoodcancerwarriors
Day 9
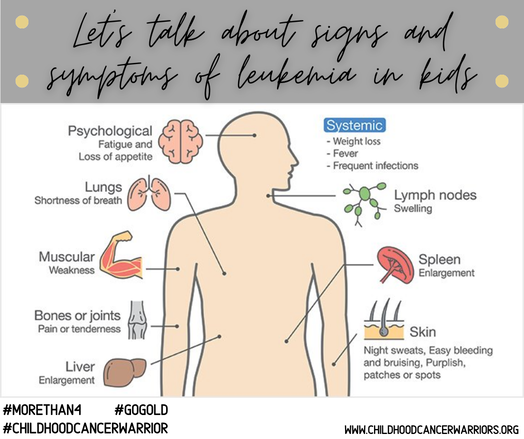
Day 9: Signs and Symptoms of Leukemia
low grade fever, fatigue, bruising, loss of appetite, colds that linger....
Sounds very normal for an active toddler to have these symptoms, right?
On March 19, 2019 we almost lost Lukas, his blood was saturated with CANCER cells called BLASTS. 75% BLASTS!! His white blood cell count was 20,000. His platelets were 38. His hemoglobin was 10.3. he spent 2 weeks in the pediatric intensive care unit, he received 3 blood transfusions, 3 platelet transfusions.
I almost lost my 21 month old baby. In one day my entire world flipped upside down, heart shattered into pieces. Lukas was diagnosed with standard Risk Acute Lymphoblastic Leukemia, he is 2.5 years into his 3.5 year cancer treatment, fighting for his life, fighting for a future.
Did you know LEUKEMIA is a BLOOD CANCER?
Did you know that Illinois is ranked 17 when it comes to overall cases per year
Did you know the current treatment for girls is 2.5 years and boys is 3.5 years of intense chemotherapy?
Did you know there are 4 risk levels, Low, Standard, High, Very High?
Did you know the common name for LEUKEMIA is the SILENT KILLER?
Did you know the initial symptoms are very mild? Low grade fever, stomachaches, fatigue, bruising.
In the United States, about 3,500 children are diagnosed with leukemia each year.
Leukemia is the most common childhood cancer, making up about a third of all pediatric cancers.
leukemia is the second leading cause of cancer death among children.
Acute Lymphoblastic Leukemia (ALL) is most common in early childhood, peaking between 2 and 5 years of age
SEPTEMBER IS BLOOD CANCER AWARENESS MONTH!
SEPTEMBER IS LEUKEMIA AWARENESS MONTH!
SEPTEMBER IS PEDIATRIC CANCER AWARENESS MONTH!!
GO GOLD!!
#journeyofaleukemiawarrior #gogoldforchildhoodcancer #childhoodcancerawareness #cancermom #childhoodcancerwarrior #pediatriccancerawareness #morethan4 #septemberischildhoodcancerawarenessmonth #gogold #BeBoldGoGold #pediatriccancer #ccam #childhoodcancerwarriors
low grade fever, fatigue, bruising, loss of appetite, colds that linger....
Sounds very normal for an active toddler to have these symptoms, right?
On March 19, 2019 we almost lost Lukas, his blood was saturated with CANCER cells called BLASTS. 75% BLASTS!! His white blood cell count was 20,000. His platelets were 38. His hemoglobin was 10.3. he spent 2 weeks in the pediatric intensive care unit, he received 3 blood transfusions, 3 platelet transfusions.
I almost lost my 21 month old baby. In one day my entire world flipped upside down, heart shattered into pieces. Lukas was diagnosed with standard Risk Acute Lymphoblastic Leukemia, he is 2.5 years into his 3.5 year cancer treatment, fighting for his life, fighting for a future.
Did you know LEUKEMIA is a BLOOD CANCER?
Did you know that Illinois is ranked 17 when it comes to overall cases per year
Did you know the current treatment for girls is 2.5 years and boys is 3.5 years of intense chemotherapy?
Did you know there are 4 risk levels, Low, Standard, High, Very High?
Did you know the common name for LEUKEMIA is the SILENT KILLER?
Did you know the initial symptoms are very mild? Low grade fever, stomachaches, fatigue, bruising.
In the United States, about 3,500 children are diagnosed with leukemia each year.
Leukemia is the most common childhood cancer, making up about a third of all pediatric cancers.
leukemia is the second leading cause of cancer death among children.
Acute Lymphoblastic Leukemia (ALL) is most common in early childhood, peaking between 2 and 5 years of age
SEPTEMBER IS BLOOD CANCER AWARENESS MONTH!
SEPTEMBER IS LEUKEMIA AWARENESS MONTH!
SEPTEMBER IS PEDIATRIC CANCER AWARENESS MONTH!!
GO GOLD!!
#journeyofaleukemiawarrior #gogoldforchildhoodcancer #childhoodcancerawareness #cancermom #childhoodcancerwarrior #pediatriccancerawareness #morethan4 #septemberischildhoodcancerawarenessmonth #gogold #BeBoldGoGold #pediatriccancer #ccam #childhoodcancerwarriors
Day 10
Day 10: Cancer Siblings
He needs a cure...for his Brother! Any questions?
Childhood cancer: two words no sibling should ever learn! An illness no family wants to endure.
50% of siblings of a child or young adult fighting cancer show signs of PTSD (post traumatic stress disorder) according to His Kids Cancer Support. For many, this can be life-long survivor guilt, depression, or addiction.
What are we doing to support them? Families often have to drive 2-4+ hours to receive specialized care for kids with cancer, so how do siblings receive the care they need? Many local counselors aren’t equipped to offer the types of sibling services required to give the care they need. Sometimes, just meeting a “friend” who has walked the same journey can offer the best support where children feel safe enough to talk openly about how they feel or what they have experienced.
Sending random cards, care packages, special trips focused on siblings without “the cancer kid” is important but difficult to do as financially strapped cancer families have other worries that take precedent. Affordable treatment, food, gas for trips, household bills, etc. all weigh heavily on parents.
Organizations like Camp One Step by Children's Oncology Services Camp Rainbow HIS KIDS Inc. for Families Affected by Childhood Cancer Leaps of Love offer opportunities to support sibling care. They especially need donor support for the TEENAGE population.
Courage isn’t just the face of a child with cancer, courage is the face of a sibling giving you the “thumbs up” hoping everything will be ok on his way to school!
National supports can be found with organizations like American Childhood Cancer Organization Gold Together for Childhood Cancer Rally Foundation for Childhood Cancer Research Momcology: Main
Check out this article I wrote about supporting siblings
http://www.journeyofaleukemiawarrior.com/.../remember-the...
#journeyofaleukemiawarrior #gogoldforchildhoodcancer #childhoodcancerawareness #cancermom #childhoodcancerwarrior #pediatriccancerawareness #morethan4 #septemberischildhoodcancerawarenessmonth #gogold #BeBoldGoGold #pediatriccancer #ccam #childhoodcancerwarriors
He needs a cure...for his Brother! Any questions?
Childhood cancer: two words no sibling should ever learn! An illness no family wants to endure.
50% of siblings of a child or young adult fighting cancer show signs of PTSD (post traumatic stress disorder) according to His Kids Cancer Support. For many, this can be life-long survivor guilt, depression, or addiction.
What are we doing to support them? Families often have to drive 2-4+ hours to receive specialized care for kids with cancer, so how do siblings receive the care they need? Many local counselors aren’t equipped to offer the types of sibling services required to give the care they need. Sometimes, just meeting a “friend” who has walked the same journey can offer the best support where children feel safe enough to talk openly about how they feel or what they have experienced.
Sending random cards, care packages, special trips focused on siblings without “the cancer kid” is important but difficult to do as financially strapped cancer families have other worries that take precedent. Affordable treatment, food, gas for trips, household bills, etc. all weigh heavily on parents.
Organizations like Camp One Step by Children's Oncology Services Camp Rainbow HIS KIDS Inc. for Families Affected by Childhood Cancer Leaps of Love offer opportunities to support sibling care. They especially need donor support for the TEENAGE population.
Courage isn’t just the face of a child with cancer, courage is the face of a sibling giving you the “thumbs up” hoping everything will be ok on his way to school!
National supports can be found with organizations like American Childhood Cancer Organization Gold Together for Childhood Cancer Rally Foundation for Childhood Cancer Research Momcology: Main
Check out this article I wrote about supporting siblings
http://www.journeyofaleukemiawarrior.com/.../remember-the...
#journeyofaleukemiawarrior #gogoldforchildhoodcancer #childhoodcancerawareness #cancermom #childhoodcancerwarrior #pediatriccancerawareness #morethan4 #septemberischildhoodcancerawarenessmonth #gogold #BeBoldGoGold #pediatriccancer #ccam #childhoodcancerwarriors
Day 11
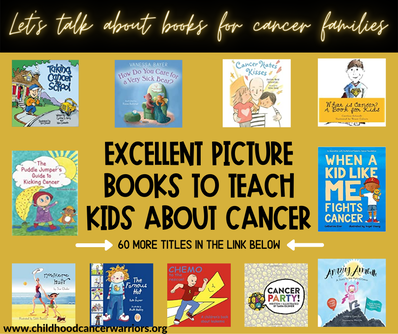
Day 11: Books about Cancer for Kids
September is National Childhood Cancer Awareness Month. It breaks my heart that we live in a world where kids get cancer, but here is a list of books for kids facing a cancer diagnosis and their families. There are over 70 books on the list to help children understand what they are going through.
https://amzn.to/35dgvCi
(I put it on amazon, so you can easily find the titles)
#picturebooksforkids #picturebooksforcancer #cancerbooksforkids #pediatriccancerbook #pediatriccancerpicturebooks #journeyofaleukemiawarrior #gogoldforchildhoodcancer #CCAM #childhoodcancerawareness #cancermom #childhoodcancerwarrior #acutelymphoblasticleukemia #acutemyeloidleukemia #Neuroblastoma #wilmstumor #sarcomaawareness #rhabdomyosarcoma #DIPG #braintumor #cancerwarrior #cancerawareness #cancerawarenessmonth #septemberischildhoodcancerawarenessmonth #ccam22
September is National Childhood Cancer Awareness Month. It breaks my heart that we live in a world where kids get cancer, but here is a list of books for kids facing a cancer diagnosis and their families. There are over 70 books on the list to help children understand what they are going through.
https://amzn.to/35dgvCi
(I put it on amazon, so you can easily find the titles)
#picturebooksforkids #picturebooksforcancer #cancerbooksforkids #pediatriccancerbook #pediatriccancerpicturebooks #journeyofaleukemiawarrior #gogoldforchildhoodcancer #CCAM #childhoodcancerawareness #cancermom #childhoodcancerwarrior #acutelymphoblasticleukemia #acutemyeloidleukemia #Neuroblastoma #wilmstumor #sarcomaawareness #rhabdomyosarcoma #DIPG #braintumor #cancerwarrior #cancerawareness #cancerawarenessmonth #septemberischildhoodcancerawarenessmonth #ccam22
Day 12
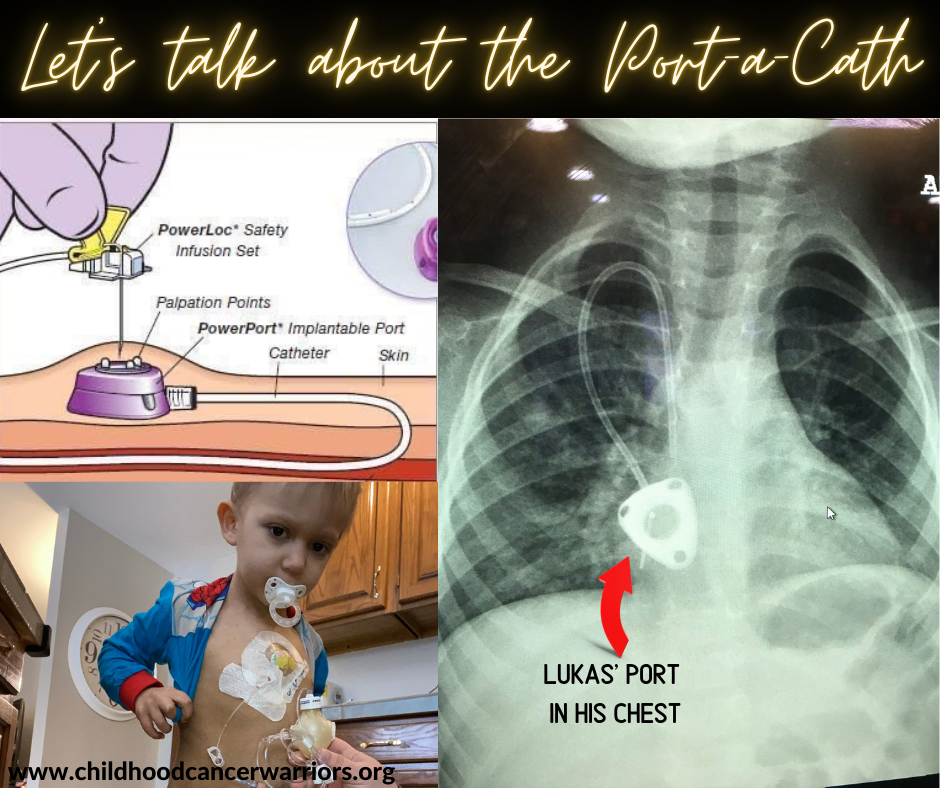
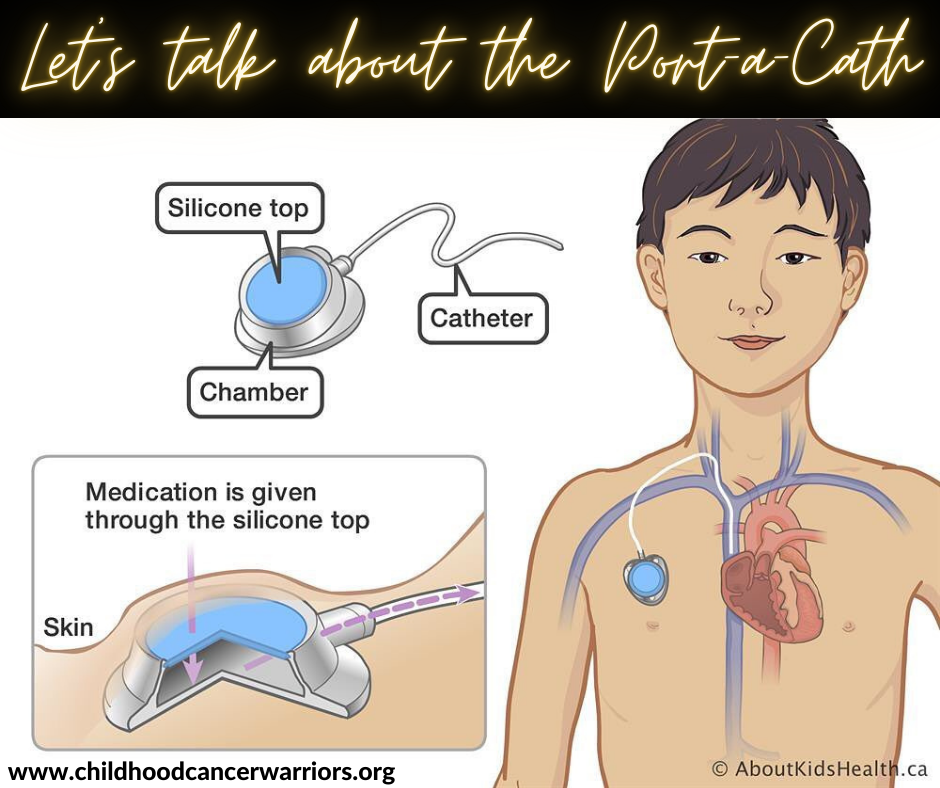
Day 12: Port-a-cath
Prior to starting chemotherapy treatments children are taken to the Operating room where a port, which is a small device placed under the skin on the right side of the chest. It is attached to a catheter (a thin, flexible tube) that is threaded into a large vein above the right side of the heart called the superior vena cava.
Ports are used for administering intravenous drugs, fluids, blood transfusions, platelets, chemotherapy, and other drugs. It is also used for taking blood samples. There is also a hickman or a broviac line that kids can get. Each one depends on the kind of cancer they have and what their treatment plan calls for.
Ports are under the skin where you can do many of your normal activities like bathing and swimming. As with a hickman or broviac, their catheters are outside of the body with the tubes hanging out. This makes bathing and swimming very difficult to impossible. Also, having your central line hanging out with tubes makes it easy for babies to pull on it and could pull it out.
Ports are under the skin where you can do many of your normal activities like bathing and swimming. As with a hickman or broviac, their catheters are outside of the body with the tubes hanging out. This makes bathing and swimming very difficult to impossible. Also, having your central line hanging out with tubes makes it easy for babies to pull on it and could pull it out.
#portacath #portacathsurgery #bloodtest #chemotherapy #cancermom #childhoodcancerwarrior #acutelymphoblasticleukemia #acutemyeloidleukemia #Neuroblastoma #wilmstumor #sarcomaawareness #rhabdomyosarcoma #DIPG #braintumor #cancerwarrior #ccam21 #journeyofaleukemiawarrior #pediatriccancer #gogold #gogoldforchildhoodcancer
Prior to starting chemotherapy treatments children are taken to the Operating room where a port, which is a small device placed under the skin on the right side of the chest. It is attached to a catheter (a thin, flexible tube) that is threaded into a large vein above the right side of the heart called the superior vena cava.
Ports are used for administering intravenous drugs, fluids, blood transfusions, platelets, chemotherapy, and other drugs. It is also used for taking blood samples. There is also a hickman or a broviac line that kids can get. Each one depends on the kind of cancer they have and what their treatment plan calls for.
Ports are under the skin where you can do many of your normal activities like bathing and swimming. As with a hickman or broviac, their catheters are outside of the body with the tubes hanging out. This makes bathing and swimming very difficult to impossible. Also, having your central line hanging out with tubes makes it easy for babies to pull on it and could pull it out.
Ports are under the skin where you can do many of your normal activities like bathing and swimming. As with a hickman or broviac, their catheters are outside of the body with the tubes hanging out. This makes bathing and swimming very difficult to impossible. Also, having your central line hanging out with tubes makes it easy for babies to pull on it and could pull it out.
#portacath #portacathsurgery #bloodtest #chemotherapy #cancermom #childhoodcancerwarrior #acutelymphoblasticleukemia #acutemyeloidleukemia #Neuroblastoma #wilmstumor #sarcomaawareness #rhabdomyosarcoma #DIPG #braintumor #cancerwarrior #ccam21 #journeyofaleukemiawarrior #pediatriccancer #gogold #gogoldforchildhoodcancer
Day 13
Day 13- Bereaved Parents
1. I wish you would not be afraid to speak my child's name. My child lived and was important and I need to hear their name.
2. If I cry or get emotional if we talk about my child, I wish you knew that it isn't because you have hurt me; the fact that my child died has caused my tears. You have allowed me to cry and thank you. Crying and emotional outbursts are healing.
3. I wish you wouldn't "kill" my child again by removing from your home their pictures, artwork, or other remembrances.
4. I will have emotional highs and lows, ups and downs. I wish you wouldn't think that if I have a good day my grief is all over, or that if I have a bad day I need psychiatric counseling.
5. I wish you knew that the death of a child is different from other losses and must be viewed separately. It is the ultimate tragedy and I wish you wouldn't compare it to your loss of a parent, a spouse, or a pet.
6. Being a bereaved parent is not contagious so I wish you wouldn't shy away from me.
7. I wish you knew all of the "crazy" grief reactions that I am having are in fact very normal. Depression, anger, frustration, hopelessness, and the questioning of values and beliefs are to be expected following the death of a child.
8. I wish you wouldn't expect my grief to be over in six months. The first few years are going to be exceedingly traumatic. As with alcoholics, I will never be "cured" or a "former bereaved parent", but will forevermore be a "recovering bereaved parent".
9. I wish you understood the physical reactions to grief. I may gain weight or lose weight, sleep all the time or not at all, develop a host of illnesses and be accident-prone, all of which may be related to my grief.
10. My child's birthday, the anniversary of their death, and holidays are terrible times for me. I wish you would tell me that you are thinking about me or my child these days, and if I get quiet and withdrawn, just know that I’m thinking about my child and don't try to coerce me into being cheerful.
11. It is normal that most of us re-examine our faith, values, and beliefs after losing a child. We will question things we have been taught all our lives and hopefully come to some new understanding with our God. I wish you would let me tangle with my religion without making me feel guilty.
12. I wish you understood that grief changes people. I am not the same person I was before my child died and I never will be that person again. If you keep waiting for me to "get back to my old self", you will stay frustrated. I am a new creature with new thoughts, dreams, aspirations, values and beliefs. Please try to get to know the new me - maybe you'll still like me.
13. I wish you knew that I am not the only one hurting, my significant other, spouse, partner, children, and extended family all hurts the same. We all need the same grace and understanding.
*Thank you to all the parents out there that shared their beautiful angels with me to make this video to remind everyone how important raising awareness is to fund research to better help other children so no other family has to lose a child!
#journeyofaleukemiawarrior #gogoldforchildhoodcancer #CCAM #childhoodcancerawareness #cancermom #childhoodcancerwarrior #acutelymphoblasticleukemia #acutemyeloidleukemia #Neuroblastoma #wilmstumor #sarcomaawareness #rhabdomyosarcoma #DIPG #braintumor #cancerwarrior #cancerawareness #cancerawarenessmonth #septemberischildhoodcancerawarenessmonth #CCAM21 #gogold #morethan4 #duckprints #pediatriccancer #leukemiawarrior
1. I wish you would not be afraid to speak my child's name. My child lived and was important and I need to hear their name.
2. If I cry or get emotional if we talk about my child, I wish you knew that it isn't because you have hurt me; the fact that my child died has caused my tears. You have allowed me to cry and thank you. Crying and emotional outbursts are healing.
3. I wish you wouldn't "kill" my child again by removing from your home their pictures, artwork, or other remembrances.
4. I will have emotional highs and lows, ups and downs. I wish you wouldn't think that if I have a good day my grief is all over, or that if I have a bad day I need psychiatric counseling.
5. I wish you knew that the death of a child is different from other losses and must be viewed separately. It is the ultimate tragedy and I wish you wouldn't compare it to your loss of a parent, a spouse, or a pet.
6. Being a bereaved parent is not contagious so I wish you wouldn't shy away from me.
7. I wish you knew all of the "crazy" grief reactions that I am having are in fact very normal. Depression, anger, frustration, hopelessness, and the questioning of values and beliefs are to be expected following the death of a child.
8. I wish you wouldn't expect my grief to be over in six months. The first few years are going to be exceedingly traumatic. As with alcoholics, I will never be "cured" or a "former bereaved parent", but will forevermore be a "recovering bereaved parent".
9. I wish you understood the physical reactions to grief. I may gain weight or lose weight, sleep all the time or not at all, develop a host of illnesses and be accident-prone, all of which may be related to my grief.
10. My child's birthday, the anniversary of their death, and holidays are terrible times for me. I wish you would tell me that you are thinking about me or my child these days, and if I get quiet and withdrawn, just know that I’m thinking about my child and don't try to coerce me into being cheerful.
11. It is normal that most of us re-examine our faith, values, and beliefs after losing a child. We will question things we have been taught all our lives and hopefully come to some new understanding with our God. I wish you would let me tangle with my religion without making me feel guilty.
12. I wish you understood that grief changes people. I am not the same person I was before my child died and I never will be that person again. If you keep waiting for me to "get back to my old self", you will stay frustrated. I am a new creature with new thoughts, dreams, aspirations, values and beliefs. Please try to get to know the new me - maybe you'll still like me.
13. I wish you knew that I am not the only one hurting, my significant other, spouse, partner, children, and extended family all hurts the same. We all need the same grace and understanding.
*Thank you to all the parents out there that shared their beautiful angels with me to make this video to remind everyone how important raising awareness is to fund research to better help other children so no other family has to lose a child!
#journeyofaleukemiawarrior #gogoldforchildhoodcancer #CCAM #childhoodcancerawareness #cancermom #childhoodcancerwarrior #acutelymphoblasticleukemia #acutemyeloidleukemia #Neuroblastoma #wilmstumor #sarcomaawareness #rhabdomyosarcoma #DIPG #braintumor #cancerwarrior #cancerawareness #cancerawarenessmonth #septemberischildhoodcancerawarenessmonth #CCAM21 #gogold #morethan4 #duckprints #pediatriccancer #leukemiawarrior
Day 14
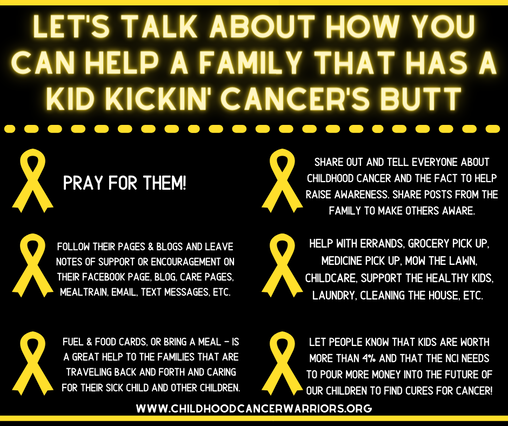
Day 14: How to Help a Cancer Family
The first few days, weeks, months are a huge blur to a cancer family. They are scared, nervous, overwhelmed, angry, sad, and a whole bunch of other emotions. The only thing that is on the forefront of their mind is how they are going to save their child from cancer.
Everything else gets pushed to the back burner to get done. Some days its just a triumph that you get out of bed in the morning.
Bills, groceries, errands, chores, just don't get done. Add that to the growing pile of worry that a cancer family has and it can just become too much!
Everyone in the beginning wants to know what they can do to help. Here are some great ideas that can majorly support cancer families as they focus their attention to the battle they are all fighting.
Remember, just because they look like they are getting better doesn't mean the fight is over. Cancer families need continuous support THROUGHOUT their journey not just in the beginning.
Don't just say you want to help -- DO SOMETHING!
Check out this article I wrote about supporting siblings
http://www.journeyofaleukemiawarrior.com/.../real-talk-6...
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogold #makeseptembergold #childhoodcancer #pediatriccancerawareness #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #gogoldforchildhoodcancer #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
The first few days, weeks, months are a huge blur to a cancer family. They are scared, nervous, overwhelmed, angry, sad, and a whole bunch of other emotions. The only thing that is on the forefront of their mind is how they are going to save their child from cancer.
Everything else gets pushed to the back burner to get done. Some days its just a triumph that you get out of bed in the morning.
Bills, groceries, errands, chores, just don't get done. Add that to the growing pile of worry that a cancer family has and it can just become too much!
Everyone in the beginning wants to know what they can do to help. Here are some great ideas that can majorly support cancer families as they focus their attention to the battle they are all fighting.
Remember, just because they look like they are getting better doesn't mean the fight is over. Cancer families need continuous support THROUGHOUT their journey not just in the beginning.
Don't just say you want to help -- DO SOMETHING!
Check out this article I wrote about supporting siblings
http://www.journeyofaleukemiawarrior.com/.../real-talk-6...
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogold #makeseptembergold #childhoodcancer #pediatriccancerawareness #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #gogoldforchildhoodcancer #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
Day 15
Day 15: On Wednesday's we Wear GOLD!
Even the Mean Girls know what is up!
Be Bold - Wear Gold!
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #duckprints #gogold #makeseptembergold #childhoodcancer #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
Even the Mean Girls know what is up!
Be Bold - Wear Gold!
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #duckprints #gogold #makeseptembergold #childhoodcancer #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
Day 16
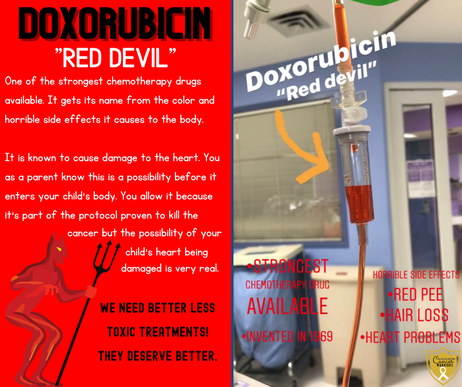
Day 16: Doxorubicin— “Red Devil”
This is one of the strongest chemo drugs that children receive. It has absolutely terrible and awful side effects.
One of the major side effects is heart failure. Prior to starting this drug a child will receive an EKG to make sure they have a baseline of their heart function. Every year cancer kids will have an EKG to make sure there’s been no damage to their heart.
This is just one of the many side effects that they will have to face after treatment is done.
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #duckprints #gogold #makeseptembergold #childhoodcancer #pediatriccancerawareness #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #gogoldforchildhoodcancer #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting
This is one of the strongest chemo drugs that children receive. It has absolutely terrible and awful side effects.
One of the major side effects is heart failure. Prior to starting this drug a child will receive an EKG to make sure they have a baseline of their heart function. Every year cancer kids will have an EKG to make sure there’s been no damage to their heart.
This is just one of the many side effects that they will have to face after treatment is done.
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #duckprints #gogold #makeseptembergold #childhoodcancer #pediatriccancerawareness #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #gogoldforchildhoodcancer #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting
Day 17
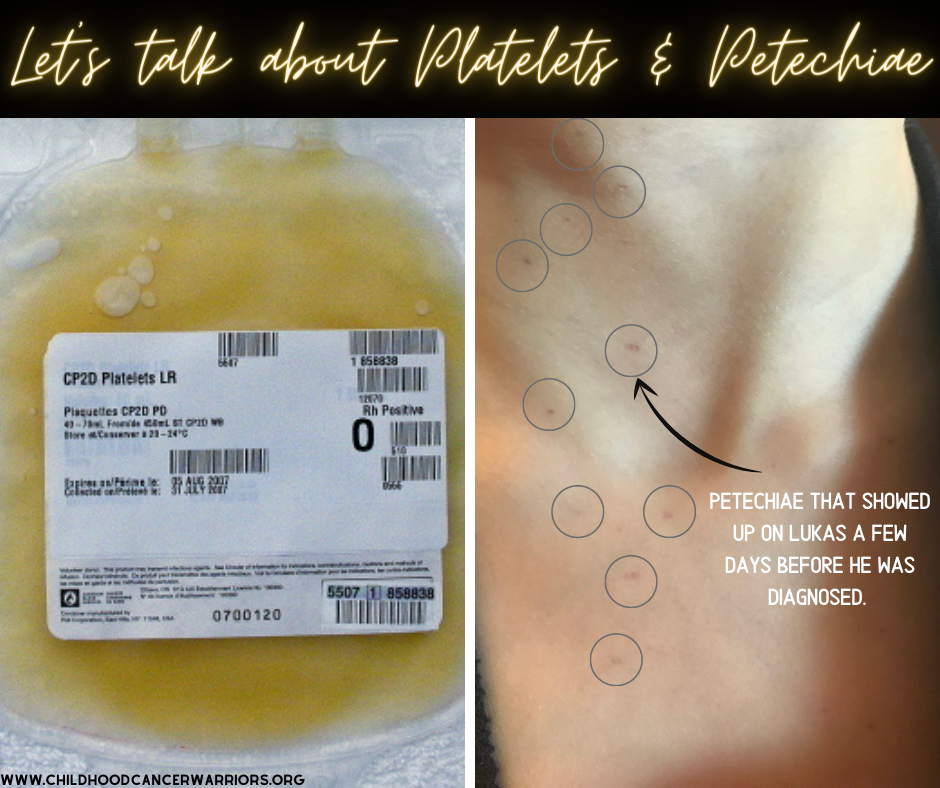
Day 17: Platelets and Petechiae
PETECHIAE - LOW PLATELETS RASH
Many people have not heard of platelets and know what their job is in your body.
Platelets (or thrombocytes) are colorless blood cells that help blood clot.
A sign of low platelets is a rash called PETECHIAE.
When your skin is injured or broken, platelets clump together and form clots to stop the bleeding. When you don't have enough platelets in your blood, your body can't form clots and “excessive bleeding” can occur. This can have serious complications in some cases.
Petechiae is one of the signs of a low platelet count. It is superficial bleeding into the skin that appears as a rash of pinpoint-sized reddish-purple spots. It often presents on the lower legs but, can be anywhere really.
PETECHIAE can sometimes be a sign of a blood cancer like leukemia, not always but, sometimes. It can also be caused by many other medical conditions. The only sign/symptom that Lukas presented before getting diagnosed was having a little red dots on his neck and torso.
One of the many results that parents get when their kids have "counts" is their platelet count. They also get ANC and HGB. These three are the magic numbers to tell you how things are going inside your kids body. If their platelet count is low (75 or less) they will need to receive a platelet transfusion.
Before the transfusion starts a set of observations are taken of blood pressure, temperature, pulse and respiratory rate. These observations are taken regularly throughout the transfusion and then at the end. These are taken in case of a reaction to the transfusion; reactions can include shivering, a rise in temperature, itching or a skin rash. If any of these symptoms occur the transfusion may be stopped and the symptoms treated.
Know the signs and symptoms of childhood cancer.
Be aware!
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #duckprints #gogold #makeseptembergold #childhoodcancer #pediatriccancerawareness #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #gogoldforchildhoodcancer #childhoodcancerwarriors #pediatriccancer #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting
PETECHIAE - LOW PLATELETS RASH
Many people have not heard of platelets and know what their job is in your body.
Platelets (or thrombocytes) are colorless blood cells that help blood clot.
A sign of low platelets is a rash called PETECHIAE.
When your skin is injured or broken, platelets clump together and form clots to stop the bleeding. When you don't have enough platelets in your blood, your body can't form clots and “excessive bleeding” can occur. This can have serious complications in some cases.
Petechiae is one of the signs of a low platelet count. It is superficial bleeding into the skin that appears as a rash of pinpoint-sized reddish-purple spots. It often presents on the lower legs but, can be anywhere really.
PETECHIAE can sometimes be a sign of a blood cancer like leukemia, not always but, sometimes. It can also be caused by many other medical conditions. The only sign/symptom that Lukas presented before getting diagnosed was having a little red dots on his neck and torso.
One of the many results that parents get when their kids have "counts" is their platelet count. They also get ANC and HGB. These three are the magic numbers to tell you how things are going inside your kids body. If their platelet count is low (75 or less) they will need to receive a platelet transfusion.
Before the transfusion starts a set of observations are taken of blood pressure, temperature, pulse and respiratory rate. These observations are taken regularly throughout the transfusion and then at the end. These are taken in case of a reaction to the transfusion; reactions can include shivering, a rise in temperature, itching or a skin rash. If any of these symptoms occur the transfusion may be stopped and the symptoms treated.
Know the signs and symptoms of childhood cancer.
Be aware!
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #duckprints #gogold #makeseptembergold #childhoodcancer #pediatriccancerawareness #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #gogoldforchildhoodcancer #childhoodcancerwarriors #pediatriccancer #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting
Day 18
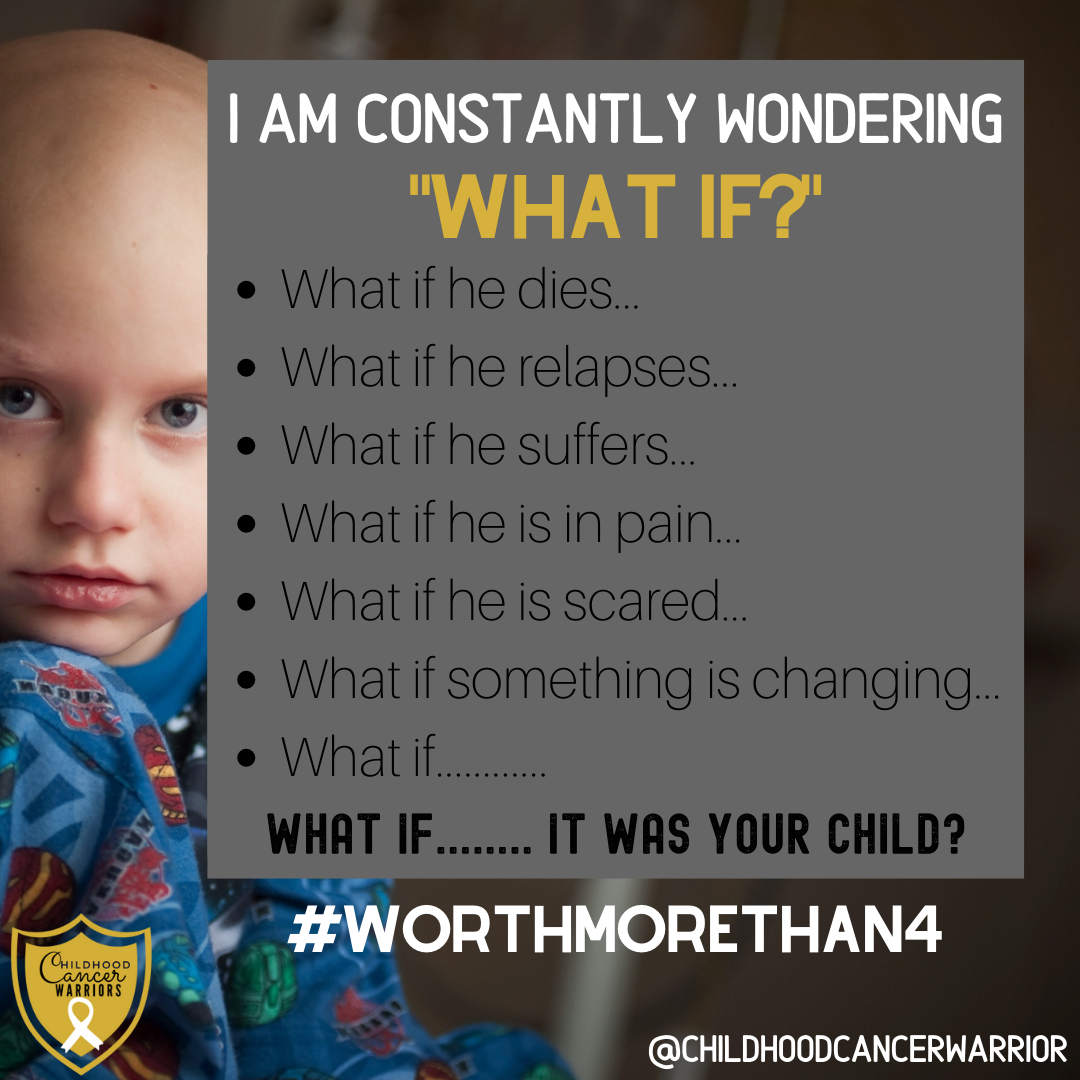
Day 18: “What if….”
As a cancer mom or parent I have these thoughts each and every day. I don’t think I’ll ever stop thinking like this.
I hate how cancer has made me have constant worries and anxiety. I will never be the mom or person I was the day before Lukas was diagnosed. For 914 days I have had these thoughts run through my mind daily.
Unless you are a cancer family you will never know or understand the deep, sickening, feeling or worry and sadness. I never wish this in anyone!
We need to do better! No family should feel like this!
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogold #makeseptembergold #childhoodcancer #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
As a cancer mom or parent I have these thoughts each and every day. I don’t think I’ll ever stop thinking like this.
I hate how cancer has made me have constant worries and anxiety. I will never be the mom or person I was the day before Lukas was diagnosed. For 914 days I have had these thoughts run through my mind daily.
Unless you are a cancer family you will never know or understand the deep, sickening, feeling or worry and sadness. I never wish this in anyone!
We need to do better! No family should feel like this!
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogold #makeseptembergold #childhoodcancer #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
Day 19
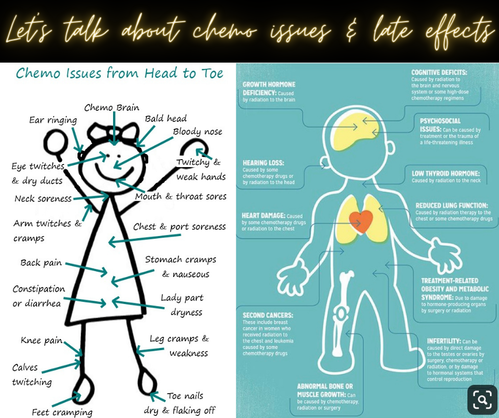
Day 19: What Causes Late Effects?
The cancer itself is not what usually causes the late effects — rather, it's the treatment. Chemotherapy and radiation both work by killing fast-growing cells. Cancer cells are among those, but unfortunately so are lots of other healthy cells.
More research needs to be done to fully understand how late effects happen so severely and consistently with children. Researchers think it is likely that damage to the cells at critical points in a child's development leads to late effects.
Ten Late Effects of Childhood Cancer treatment
1. Heart problems.
Kids who had chest radiation and/or chemo with a class of drugs called anthracycline ( one of which is the infamous Doxorubicin) are at higher risk for heart problems up to 20 years or longer after treatment. The severity of the problem depends on how much chemo and/or chest radiation they got and the child's age during treatment.
2. Thyroid problems.
The thyroid is a gland of the endocrine system that controls metabolism (chemical reactions in the body's cells). It may be damaged by radiation to the head or neck. The result is typically hypothyroidism (when the thyroid doesn't make enough thyroid hormone), leading to tiredness, weight gain, thinning hair, and dry skin.
3. Hearing loss.
Chemotherapy, radiation to the brain, and even some antibiotics can lead to high-frequency hearing loss (when a person cannot hear high-pitched sounds), tinnitus (ringing in the ears), or dizziness.
4. Learning problems.
Some chemotherapy drugs and/or radiation to the brain may interfere with learning. The problems can range from mild to severe, and may show up during treatment, soon after treatment, or several years later. Common learning problems include problems with memory, processing speed, and multi-tasking.
5. Lung, liver, or kidney problems.
Childhood cancer treatments have been linked to several types of body organ damage later in life. How serious the organ damage is depends on the type of cancer and treatment.
6. Dental problems.
Short dental roots, delayed teeth, or missing teeth are more common in very young children who've had radiation to the brain and/or chemotherapy with a drug called vincristine. All kids who have had chemo are at risk for tooth decay and gum disease.
7. Vision problems.
Blurred or double vision, glaucoma, or cataracts are more likely in kids who were treated for tumors near the eye or received radiation to the brain.
8. Abnormal bone growth.
Sometimes kids do not grow in the usual timeframe and/or stop growing much earlier than normal. This may be due to radiation treatment, chemotherapy, or a brain tumor or its treatment. Kids may also be at risk for developing osteoporosis (bone thinning) or scoliosis (a curved spine).
9. Increased risk of future cancers.
Childhood cancer survivors have a higher risk of developing a second cancer at some point — even if the original cancer doesn't come back
10. Fertility issues and delayed sexual development
Both chemotherapy and radiation can cause fertility problems and sexual development issues.
Studies of the causes of late effects have led to changes in treatment. This has improved the quality of life for cancer survivors and helps prevent illness and death from late effects.
WE NEED MORE RESEARCH AND KINDER TREATMENTS
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogold #makeseptembergold #childhoodcancer #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
The cancer itself is not what usually causes the late effects — rather, it's the treatment. Chemotherapy and radiation both work by killing fast-growing cells. Cancer cells are among those, but unfortunately so are lots of other healthy cells.
More research needs to be done to fully understand how late effects happen so severely and consistently with children. Researchers think it is likely that damage to the cells at critical points in a child's development leads to late effects.
Ten Late Effects of Childhood Cancer treatment
1. Heart problems.
Kids who had chest radiation and/or chemo with a class of drugs called anthracycline ( one of which is the infamous Doxorubicin) are at higher risk for heart problems up to 20 years or longer after treatment. The severity of the problem depends on how much chemo and/or chest radiation they got and the child's age during treatment.
2. Thyroid problems.
The thyroid is a gland of the endocrine system that controls metabolism (chemical reactions in the body's cells). It may be damaged by radiation to the head or neck. The result is typically hypothyroidism (when the thyroid doesn't make enough thyroid hormone), leading to tiredness, weight gain, thinning hair, and dry skin.
3. Hearing loss.
Chemotherapy, radiation to the brain, and even some antibiotics can lead to high-frequency hearing loss (when a person cannot hear high-pitched sounds), tinnitus (ringing in the ears), or dizziness.
4. Learning problems.
Some chemotherapy drugs and/or radiation to the brain may interfere with learning. The problems can range from mild to severe, and may show up during treatment, soon after treatment, or several years later. Common learning problems include problems with memory, processing speed, and multi-tasking.
5. Lung, liver, or kidney problems.
Childhood cancer treatments have been linked to several types of body organ damage later in life. How serious the organ damage is depends on the type of cancer and treatment.
6. Dental problems.
Short dental roots, delayed teeth, or missing teeth are more common in very young children who've had radiation to the brain and/or chemotherapy with a drug called vincristine. All kids who have had chemo are at risk for tooth decay and gum disease.
7. Vision problems.
Blurred or double vision, glaucoma, or cataracts are more likely in kids who were treated for tumors near the eye or received radiation to the brain.
8. Abnormal bone growth.
Sometimes kids do not grow in the usual timeframe and/or stop growing much earlier than normal. This may be due to radiation treatment, chemotherapy, or a brain tumor or its treatment. Kids may also be at risk for developing osteoporosis (bone thinning) or scoliosis (a curved spine).
9. Increased risk of future cancers.
Childhood cancer survivors have a higher risk of developing a second cancer at some point — even if the original cancer doesn't come back
10. Fertility issues and delayed sexual development
Both chemotherapy and radiation can cause fertility problems and sexual development issues.
Studies of the causes of late effects have led to changes in treatment. This has improved the quality of life for cancer survivors and helps prevent illness and death from late effects.
WE NEED MORE RESEARCH AND KINDER TREATMENTS
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogold #makeseptembergold #childhoodcancer #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
Day 20
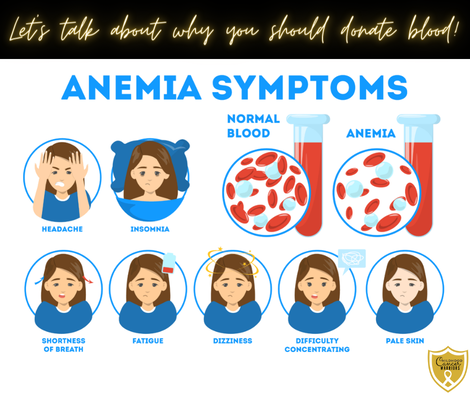
Day 20: Blood Transfusions
Many people aren't aware that children on cancer treatment (in fact any cancer patient really) will likely need multiple blood transfusions. Lukas has had 6 transfusions.
This is because some cancer treatments reduce the number of red blood cells, causing anemia. Chemotherapy and sometimes radiation can affect the levels of the red blood cells in the blood and if they become too low then a transfusion will be necessary.
Anemia can cause feelings of fatigue, pale skin, heart problems, dizziness, cold hands and feet and breathlessness. Anemia is a condition in which you lack enough healthy red blood cells to carry adequate oxygen to your body's tissues. Having anemia, can also be referred to as low hemoglobin.
Many children need at least 1 blood transfusion on each chemo cycle, some need more - this can run into many many blood transfusions over time.
The effects of a transfusion can be incredible and sometimes instantaneous, with energy levels increasing and fatigue levels decreasing to normal levels.
All these children depend on the kindness of strangers for donating their blood. Blood donors are, quite literally, life savers.
If you can, please donate blood (or platelets) -- Oncology parents thank you!
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogold #makeseptembergold #childhoodcancer #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
Many people aren't aware that children on cancer treatment (in fact any cancer patient really) will likely need multiple blood transfusions. Lukas has had 6 transfusions.
This is because some cancer treatments reduce the number of red blood cells, causing anemia. Chemotherapy and sometimes radiation can affect the levels of the red blood cells in the blood and if they become too low then a transfusion will be necessary.
Anemia can cause feelings of fatigue, pale skin, heart problems, dizziness, cold hands and feet and breathlessness. Anemia is a condition in which you lack enough healthy red blood cells to carry adequate oxygen to your body's tissues. Having anemia, can also be referred to as low hemoglobin.
Many children need at least 1 blood transfusion on each chemo cycle, some need more - this can run into many many blood transfusions over time.
The effects of a transfusion can be incredible and sometimes instantaneous, with energy levels increasing and fatigue levels decreasing to normal levels.
All these children depend on the kindness of strangers for donating their blood. Blood donors are, quite literally, life savers.
If you can, please donate blood (or platelets) -- Oncology parents thank you!
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogold #makeseptembergold #childhoodcancer #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
To illustrate just how important blood transfusions are to children on cancer treatment, how lifesaving they are and how frequently they are needed, please tell us how many your child, teen or young adult has had?
Day 21
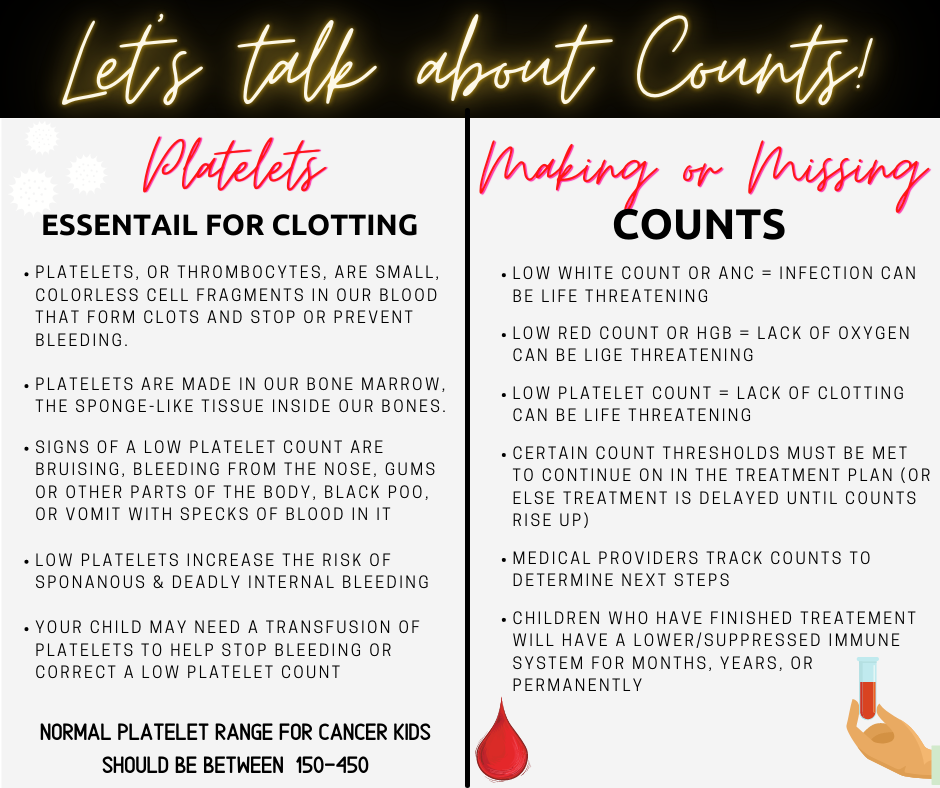
Day 21: Counts
You’ll likely hear cancer families talk about COUNTS — typically in the context of “making” counts or not.
Counts are taken before each round of chemotherapy (or any procedure) to determine if a child's body is ready for more treatment. Minimum thresholds must be met to receive chemotherapy, or treatment is delayed. Delays for missed counts are common, but stressful.
You need to give the body time to rebound. But you also don’t want to give the cancer cells time to rebound.
When counts are low, a child's body can’t defend itself or heal itself properly -- so everything from a skinned knee to houseplants become a threat. (cancer families are told to give away their houseplants at the start of treatment, because possible mold spores could cause an infection in a neutropenic person)
It’s stressful to families because it’s unpredictable. Are we being admitted for 5 days of inpatient chemo? Or are we going home and trying again in 3 days?
When counts are low, everything stops. Cancer can can't go to school. Be in public. Miss out on activities, etc. We have to keep our kids safe and away from germs. Their bodies do not what it needs to fight off infections.
Blood and platelets transfusions are common to address critically low counts, but they can’t be used to push a kid over the threshold to “make counts” for treatment. A kid's body has to show that he/she is rebounding.
One of the many ways you can support a cancer warrior is to donate blood. And if you get to hang around a warrior, observe good hand-hygiene, vaccines, and masks are also important. Your sniffles may be no big deal to you, but it could send a cancer kid racing to the emergency room.
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogold #makeseptembergold #childhoodcancer #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
You’ll likely hear cancer families talk about COUNTS — typically in the context of “making” counts or not.
Counts are taken before each round of chemotherapy (or any procedure) to determine if a child's body is ready for more treatment. Minimum thresholds must be met to receive chemotherapy, or treatment is delayed. Delays for missed counts are common, but stressful.
You need to give the body time to rebound. But you also don’t want to give the cancer cells time to rebound.
When counts are low, a child's body can’t defend itself or heal itself properly -- so everything from a skinned knee to houseplants become a threat. (cancer families are told to give away their houseplants at the start of treatment, because possible mold spores could cause an infection in a neutropenic person)
It’s stressful to families because it’s unpredictable. Are we being admitted for 5 days of inpatient chemo? Or are we going home and trying again in 3 days?
When counts are low, everything stops. Cancer can can't go to school. Be in public. Miss out on activities, etc. We have to keep our kids safe and away from germs. Their bodies do not what it needs to fight off infections.
Blood and platelets transfusions are common to address critically low counts, but they can’t be used to push a kid over the threshold to “make counts” for treatment. A kid's body has to show that he/she is rebounding.
One of the many ways you can support a cancer warrior is to donate blood. And if you get to hang around a warrior, observe good hand-hygiene, vaccines, and masks are also important. Your sniffles may be no big deal to you, but it could send a cancer kid racing to the emergency room.
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogold #makeseptembergold #childhoodcancer #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
Day 22
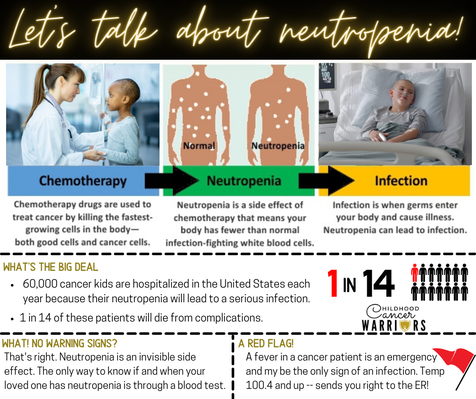
Day 22: Neutropenia
Children, teens and young adults have chemotherapy as part of their treatment. During this treatment they are at risk of a potentially fatal complication called neutropenic sepsis.
Neutropenia is a blood condition characterized by low levels of neutrophils, which are white blood cells that protect your body from infections. Without enough neutrophils, your body can't fight off bacteria. Having neutropenia increases your risk for many types of infection.
As parents we check our children's temperature constantly and are never too far from a thermometer. If their temperature goes above 100.4 degrees it means an urgent trip to hospital, a minimum of a three day admission hooked up to intravenous antibiotics and needing regular blood tests.
This happens EVERY time a cancer kid spikes a temperature... EVERY TIME!
Please help us protect our children by ensuring you keep your sick children at home while they're recovering. Our kids rely on your to help keep them healthy and out of the hospital.
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogold #makeseptembergold #childhoodcancer #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
Children, teens and young adults have chemotherapy as part of their treatment. During this treatment they are at risk of a potentially fatal complication called neutropenic sepsis.
Neutropenia is a blood condition characterized by low levels of neutrophils, which are white blood cells that protect your body from infections. Without enough neutrophils, your body can't fight off bacteria. Having neutropenia increases your risk for many types of infection.
As parents we check our children's temperature constantly and are never too far from a thermometer. If their temperature goes above 100.4 degrees it means an urgent trip to hospital, a minimum of a three day admission hooked up to intravenous antibiotics and needing regular blood tests.
This happens EVERY time a cancer kid spikes a temperature... EVERY TIME!
Please help us protect our children by ensuring you keep your sick children at home while they're recovering. Our kids rely on your to help keep them healthy and out of the hospital.
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogold #makeseptembergold #childhoodcancer #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
Day 23
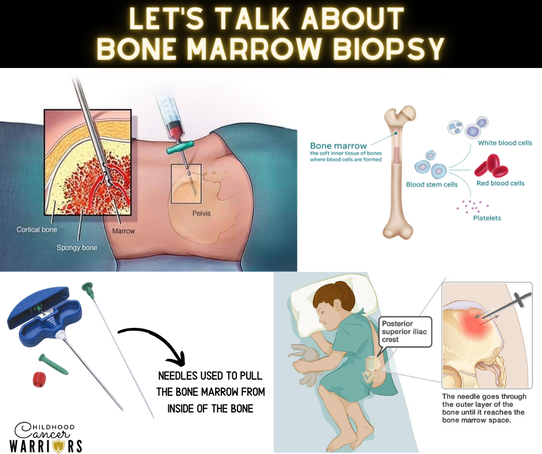
Day 23: Bone Marrow Biopsy
A bone marrow biopsy involves removing a small sample of the bone marrow inside your bones for testing. Bone marrow is a soft tissue in the center of most large bones. It makes most of the body's blood cells. The biopsy is done using a small needle inserted into the bone.
The bone marrow is part of our immune system which protects us from infection and disease. It is found inside bones, mainly the hip and breast bones and is where our stem cells are made.
Stem cells are blood cells at the earliest stage of their development and all our blood cells develop from stem cells in the bone marrow.
Stem cells stay inside the bone marrow until they are fully developed and are released into the blood stream.
The blood stem cells need to produce exactly the right balance of each type of blood cells and if that goes wrong it can lead to too many cells that are not fully developed. This can then lead to blood cancers such as leukemia and lymphoma.
A bone marrow biopsy is a test that involves taking a sample of bone marrow to be examined under a microscope looking for any healthy or unhealthy cells, such as leukemia or lymphoma cells. It is an important test to help diagnose and monitor treatment in a number of medical conditions.
Bone marrow tests are usually carried out under general anesthetic in young children and babies , however, they can be performed using a local anesthetic in teens and young adults. A hollow needle is inserted into the bone, usually the top of the pelvis.
Following the test the area around the biopsy site may be sore and bruised and there is a very small risk that the biopsy site could become infected.
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogold #makeseptembergold #childhoodcancer #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
A bone marrow biopsy involves removing a small sample of the bone marrow inside your bones for testing. Bone marrow is a soft tissue in the center of most large bones. It makes most of the body's blood cells. The biopsy is done using a small needle inserted into the bone.
The bone marrow is part of our immune system which protects us from infection and disease. It is found inside bones, mainly the hip and breast bones and is where our stem cells are made.
Stem cells are blood cells at the earliest stage of their development and all our blood cells develop from stem cells in the bone marrow.
Stem cells stay inside the bone marrow until they are fully developed and are released into the blood stream.
The blood stem cells need to produce exactly the right balance of each type of blood cells and if that goes wrong it can lead to too many cells that are not fully developed. This can then lead to blood cancers such as leukemia and lymphoma.
A bone marrow biopsy is a test that involves taking a sample of bone marrow to be examined under a microscope looking for any healthy or unhealthy cells, such as leukemia or lymphoma cells. It is an important test to help diagnose and monitor treatment in a number of medical conditions.
Bone marrow tests are usually carried out under general anesthetic in young children and babies , however, they can be performed using a local anesthetic in teens and young adults. A hollow needle is inserted into the bone, usually the top of the pelvis.
Following the test the area around the biopsy site may be sore and bruised and there is a very small risk that the biopsy site could become infected.
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogold #makeseptembergold #childhoodcancer #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
Day 24
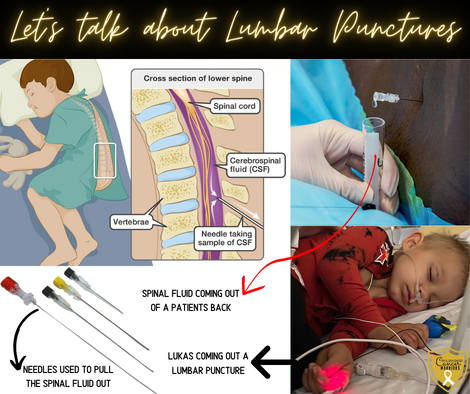
Day 24: Lumber Punctures (Spinal Taps)
A lumbar puncture (LP) or spinal tap may be done to diagnose or treat a condition. For this procedure, your healthcare provider inserts a hollow needle into the space surrounding the spinal column (subarachnoid space) in the lower back to withdraw some cerebrospinal fluid (CSF) or inject medicine.
Not only does Lukas' protocol call for several spinal tap throughout the treatment, but he also gets chemo injected right into his spinal column and his brain to prevent he leukemia from going into his CNS (central nervous system).
A lumbar puncture can help diagnose cancers of the brain or spinal cord and blood cancers such as leukemia or lymphoma. Cancer cells can pass into the fluid that surrounds the brain and spinal cord, cerebrospinal fluid or CSF which is the fluid that surrounds the brain and spinal cord to protect them from injury.
Children and young people with acute lymphoblastic leukemia (ALL) require many lumbar punctures throughout their treatment with younger children always having a general anesthetic for the LP as keeping still is very important. However, some older children and young adults may choose to have their lumbar punctures under local anesthetic.
The procedure is usually performed with the child on their side with the knees drawn up to their chest, this position flexes the back, widening the spaces between the vertebrae making it easier to insert the needle into the correct place.
Lumbar punctures are sterile procedures that involve inserting a fine needle between two vertebral bones in the lower part of the spine. A few drops of the CSF removed and then examined to see if any cancer cells are present. Lumbar punctures can also be used to diagnose infections and in the diagnosis of non cancerous conditions.
Sometimes, as part of the cancer treatment, drugs are injected into the CSF. This is known as intrathecal chemotherapy and requires a LP to be performed to gain access to the CSF.
Although lumbar punctures are generally recognized as safe, they do carry some risks.
• Post-lumbar puncture headache
• Back discomfort or pain.
• Bleeding. Bleeding may occur near the puncture site or, rarely, into the epidural space.
• Brainstem herniation. Increased pressure within the skull (intracranial), due to a brain tumor or other space-occupying lesion, can lead to compression of the brainstem after a sample of cerebrospinal fluid is removed.
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogold #makeseptembergold #childhoodcancer #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
A lumbar puncture (LP) or spinal tap may be done to diagnose or treat a condition. For this procedure, your healthcare provider inserts a hollow needle into the space surrounding the spinal column (subarachnoid space) in the lower back to withdraw some cerebrospinal fluid (CSF) or inject medicine.
Not only does Lukas' protocol call for several spinal tap throughout the treatment, but he also gets chemo injected right into his spinal column and his brain to prevent he leukemia from going into his CNS (central nervous system).
A lumbar puncture can help diagnose cancers of the brain or spinal cord and blood cancers such as leukemia or lymphoma. Cancer cells can pass into the fluid that surrounds the brain and spinal cord, cerebrospinal fluid or CSF which is the fluid that surrounds the brain and spinal cord to protect them from injury.
Children and young people with acute lymphoblastic leukemia (ALL) require many lumbar punctures throughout their treatment with younger children always having a general anesthetic for the LP as keeping still is very important. However, some older children and young adults may choose to have their lumbar punctures under local anesthetic.
The procedure is usually performed with the child on their side with the knees drawn up to their chest, this position flexes the back, widening the spaces between the vertebrae making it easier to insert the needle into the correct place.
Lumbar punctures are sterile procedures that involve inserting a fine needle between two vertebral bones in the lower part of the spine. A few drops of the CSF removed and then examined to see if any cancer cells are present. Lumbar punctures can also be used to diagnose infections and in the diagnosis of non cancerous conditions.
Sometimes, as part of the cancer treatment, drugs are injected into the CSF. This is known as intrathecal chemotherapy and requires a LP to be performed to gain access to the CSF.
Although lumbar punctures are generally recognized as safe, they do carry some risks.
• Post-lumbar puncture headache
• Back discomfort or pain.
• Bleeding. Bleeding may occur near the puncture site or, rarely, into the epidural space.
• Brainstem herniation. Increased pressure within the skull (intracranial), due to a brain tumor or other space-occupying lesion, can lead to compression of the brainstem after a sample of cerebrospinal fluid is removed.
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogold #makeseptembergold #childhoodcancer #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
Day 25
Day 25: Neuropathy
Your nervous system is divided into two parts—your central nervous system and your peripheral nervous system.
Your central nervous system consists of your brain and spinal cord. Your peripheral nervous system consists of all the nerves that are located outside of your brain and spinal cord. The function of peripheral nerves is to relay messages from your brain and spinal cord to the rest of your body, such as your arms, hands, legs, feet, internal organs, skin, and joints.
Since the peripheral nerves are not protected by the skull (as the brain is) or the vertebral spinal canal (as the spinal cord is), they are vulnerable to damage. When this happens to one or more peripheral nerves, peripheral neuropathy develops.
When one or more of these nerves become damaged—as a result of an underlying disease process, medication, or infection, to name a few possibilities—a condition called peripheral neuropathy develops.
Cancer or its treatment can cause peripheral neuropathy.
The symptoms of peripheral neuropathy vary depending upon what nerves are affected. Children can experience: Pain, burning or tingling in hands or feet.
Some of the chemotherapy and other drugs used to treat cancer can damage peripheral nerves. When this happens it is called chemotherapy-induced peripheral neuropathy (CIPN). This can be a disabling side effect of cancer treatment.
Across all ages, peripheral neuropathy causes weakness, odd sensations, and changes in motor skills such as walking, running, jumping and balance.
When children are no longer receiving the chemotherapy that caused neuropathy, symptoms typically start to improve. However, some children do have lasting effects of CIPN. A 2012 research study found that 15% of long-term childhood cancer survivors had balance deficits.
Children usually start to show symptoms of CIPN during the phase of treatment when they get the most vincristine. For Acute Lymphoblastic Leukemia, this is Interim Maintenance and Delayed Intensification. CIPN can occur at any time during treatment.
People who have received any of the following chemotherapy drugs may be at risk:
-Vincristine
-Vinblastine
-Cisplatin
-Carboplatin
People at highest risk for peripheral neuropathy are those who have received higher doses of these drugs or combinations of these drugs.
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogold #makeseptembergold #childhoodcancer #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
Your nervous system is divided into two parts—your central nervous system and your peripheral nervous system.
Your central nervous system consists of your brain and spinal cord. Your peripheral nervous system consists of all the nerves that are located outside of your brain and spinal cord. The function of peripheral nerves is to relay messages from your brain and spinal cord to the rest of your body, such as your arms, hands, legs, feet, internal organs, skin, and joints.
Since the peripheral nerves are not protected by the skull (as the brain is) or the vertebral spinal canal (as the spinal cord is), they are vulnerable to damage. When this happens to one or more peripheral nerves, peripheral neuropathy develops.
When one or more of these nerves become damaged—as a result of an underlying disease process, medication, or infection, to name a few possibilities—a condition called peripheral neuropathy develops.
Cancer or its treatment can cause peripheral neuropathy.
The symptoms of peripheral neuropathy vary depending upon what nerves are affected. Children can experience: Pain, burning or tingling in hands or feet.
Some of the chemotherapy and other drugs used to treat cancer can damage peripheral nerves. When this happens it is called chemotherapy-induced peripheral neuropathy (CIPN). This can be a disabling side effect of cancer treatment.
Across all ages, peripheral neuropathy causes weakness, odd sensations, and changes in motor skills such as walking, running, jumping and balance.
When children are no longer receiving the chemotherapy that caused neuropathy, symptoms typically start to improve. However, some children do have lasting effects of CIPN. A 2012 research study found that 15% of long-term childhood cancer survivors had balance deficits.
Children usually start to show symptoms of CIPN during the phase of treatment when they get the most vincristine. For Acute Lymphoblastic Leukemia, this is Interim Maintenance and Delayed Intensification. CIPN can occur at any time during treatment.
People who have received any of the following chemotherapy drugs may be at risk:
-Vincristine
-Vinblastine
-Cisplatin
-Carboplatin
People at highest risk for peripheral neuropathy are those who have received higher doses of these drugs or combinations of these drugs.
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogold #makeseptembergold #childhoodcancer #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
Day 26
Day 26: Chemo Toxicity
Chemotherapy drugs are used to treat cancer. However, while the purpose of chemotherapy medications is to reduce your cancer symptoms and lengthen your life, the drugs can also have unwanted effects on your body. Chemotherapy can poison your body and lead to harm, and this is known as chemotherapy toxicity.
Six Kinds of Chemotherapy Toxicity
Chemotherapy drugs work in different ways and have diverse effects on the body. Some examples of chemotherapy toxicity include:
1.Cardiac Toxicity. Some chemotherapy drugs can cause either acute or chronic toxicity to the heart. In some cases, heart failure may occur.
2. Dermatologic toxicity. Skin and nail changes may not be the most severe type of chemotherapy toxicity, but they can be uncomfortable and require medical treatment.
3. Gastrointestinal toxicity. Different types of digestive upset are common for many chemotherapy patients and may be a form of chemotherapy toxicity.
4. Hepatotoxicity. Liver toxicity caused by chemotherapy medications can be either acute or chronic.
5. Nephrotoxicity. Some chemotherapy drugs such as Cisplatin and Methotrexate can cause urinary tract toxicity or kidney problems.
6. Pulmonary toxicity. Pulmonary toxicity impacts the lungs. Supplemental oxygen and other medical interventions may be necessary to make sure that enough oxygen is received until the condition is resolved.
Generally, chemotherapy toxicity is more likely as the drug accumulates in your body. While not all instances of chemotherapy toxicity may be avoided, some cases of chemo toxicity may be prevented if the right dose of the medication is provided, and if you are regularly monitored for serious side effects.
Many side effects go away fairly quickly, but some might take months or even years to go away completely. These are called late effects. Sometimes the side effects can last a lifetime, such as when chemo causes long-term damage to the heart, lungs, kidneys, or reproductive organs.
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogold #makeseptembergold #childhoodcancer #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
Chemotherapy drugs are used to treat cancer. However, while the purpose of chemotherapy medications is to reduce your cancer symptoms and lengthen your life, the drugs can also have unwanted effects on your body. Chemotherapy can poison your body and lead to harm, and this is known as chemotherapy toxicity.
Six Kinds of Chemotherapy Toxicity
Chemotherapy drugs work in different ways and have diverse effects on the body. Some examples of chemotherapy toxicity include:
1.Cardiac Toxicity. Some chemotherapy drugs can cause either acute or chronic toxicity to the heart. In some cases, heart failure may occur.
2. Dermatologic toxicity. Skin and nail changes may not be the most severe type of chemotherapy toxicity, but they can be uncomfortable and require medical treatment.
3. Gastrointestinal toxicity. Different types of digestive upset are common for many chemotherapy patients and may be a form of chemotherapy toxicity.
4. Hepatotoxicity. Liver toxicity caused by chemotherapy medications can be either acute or chronic.
5. Nephrotoxicity. Some chemotherapy drugs such as Cisplatin and Methotrexate can cause urinary tract toxicity or kidney problems.
6. Pulmonary toxicity. Pulmonary toxicity impacts the lungs. Supplemental oxygen and other medical interventions may be necessary to make sure that enough oxygen is received until the condition is resolved.
Generally, chemotherapy toxicity is more likely as the drug accumulates in your body. While not all instances of chemotherapy toxicity may be avoided, some cases of chemo toxicity may be prevented if the right dose of the medication is provided, and if you are regularly monitored for serious side effects.
Many side effects go away fairly quickly, but some might take months or even years to go away completely. These are called late effects. Sometimes the side effects can last a lifetime, such as when chemo causes long-term damage to the heart, lungs, kidneys, or reproductive organs.
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogold #makeseptembergold #childhoodcancer #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
Day 27
Day 27: Chronic Fatigue
Cancer-related fatigue (CRF - sometimes simply called "cancer fatigue") is one of the most common side effects of cancer and its treatments. It is often described as "paralyzing." Usually, it comes on suddenly, does not result from activity or exertion, and is not relieved by rest or sleep.
Chronic fatigue is a very real and difficult side effect of cancer and it's treatment in children, teens, and young adults and is often overlooked. For some people this can have a devastating effect and cause great distress.
Some of the symptoms of chronic fatigue are:
• Lack of energy and feeling you just want to stay in bed all day
• Sleeping difficulties
• Difficulty in getting out of bed in the morning
• Anxiety, sadness, depression
• Muscle pain & difficulty walking short distances & climbing stairs
• Getting out breath easily and quickly
• Difficulty in concentrating or making decisions
• Feeling badly about yourself
Many people with these symptoms may struggle with regular attendance at their schools, colleges or place of work. It is so important that these places are aware of chronic fatigue and how it affects your day to day living so support systems can be put in place.
It affects between 70-80% of those diagnosed with cancer. For some, this can have the biggest impact after treatment finishes, and can last for weeks, months, or years.
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogold #makeseptembergold #childhoodcancer #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
Cancer-related fatigue (CRF - sometimes simply called "cancer fatigue") is one of the most common side effects of cancer and its treatments. It is often described as "paralyzing." Usually, it comes on suddenly, does not result from activity or exertion, and is not relieved by rest or sleep.
Chronic fatigue is a very real and difficult side effect of cancer and it's treatment in children, teens, and young adults and is often overlooked. For some people this can have a devastating effect and cause great distress.
Some of the symptoms of chronic fatigue are:
• Lack of energy and feeling you just want to stay in bed all day
• Sleeping difficulties
• Difficulty in getting out of bed in the morning
• Anxiety, sadness, depression
• Muscle pain & difficulty walking short distances & climbing stairs
• Getting out breath easily and quickly
• Difficulty in concentrating or making decisions
• Feeling badly about yourself
Many people with these symptoms may struggle with regular attendance at their schools, colleges or place of work. It is so important that these places are aware of chronic fatigue and how it affects your day to day living so support systems can be put in place.
It affects between 70-80% of those diagnosed with cancer. For some, this can have the biggest impact after treatment finishes, and can last for weeks, months, or years.
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogold #makeseptembergold #childhoodcancer #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
Day 28
Day 28: Chemo Brain
Many patients experience "chemobrain" — mental clouding or fogginess — during and after cancer treatment.
Symptoms generally include attention and concentration difficulties, reduced processing speed and executive function, and compromised short-term memory.
Chemo brain affects more than one-third of all survivors of childhood cancers. Children with cancer diagnosed at a young age appear to experience more chemo brain complications than any other patient group.
When a child experiences chemo brain or other cognitive deficits, keeping the mind active can help. When it comes time to introduce — or re-introduce —the child to school, slowly implementing learning can help the child feel less overwhelmed during reintegration to the school environment, as it can be a very anxiety provoking time.
A meeting with administration, teachers, and counselors prior to a classroom visit can be extremely helpful to create a plan for moving forward. Making these people aware of potential long-term adverse effects of the diagnosis and treatment is very important. A one-on-one aid or assistant for a child may be essential, and an individualized education plan (IEP) and classroom/testing accommodations (504 plan) are 2 significant requests to make. Psychological testing may also be imperative.
Once reintegration into the school environment begins, the child’s progress should be continuously monitored by parents and teachers. This allows for making necessary adjustments to accommodate changes in the child’s learning capabilities, as chemo brain may not become apparent immediately.
For most patients, chemobrain improves within 9-12 months after completing chemotherapy, but many people still have symptoms at the six-month mark. A smaller fraction of people (approximately 10-20%) may have long-term effects.
The best way to get a complete picture of your cognitive functioning is to have neuropsychological testing. Your oncologist can refer you for this evaluation. Information from neuropsychological testing can also be extremely helpful to share with your employer or school if you are hoping to get accommodations at work or extra time for exams, homework etc.
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogold #makeseptembergold #childhoodcancer #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
Many patients experience "chemobrain" — mental clouding or fogginess — during and after cancer treatment.
Symptoms generally include attention and concentration difficulties, reduced processing speed and executive function, and compromised short-term memory.
Chemo brain affects more than one-third of all survivors of childhood cancers. Children with cancer diagnosed at a young age appear to experience more chemo brain complications than any other patient group.
When a child experiences chemo brain or other cognitive deficits, keeping the mind active can help. When it comes time to introduce — or re-introduce —the child to school, slowly implementing learning can help the child feel less overwhelmed during reintegration to the school environment, as it can be a very anxiety provoking time.
A meeting with administration, teachers, and counselors prior to a classroom visit can be extremely helpful to create a plan for moving forward. Making these people aware of potential long-term adverse effects of the diagnosis and treatment is very important. A one-on-one aid or assistant for a child may be essential, and an individualized education plan (IEP) and classroom/testing accommodations (504 plan) are 2 significant requests to make. Psychological testing may also be imperative.
Once reintegration into the school environment begins, the child’s progress should be continuously monitored by parents and teachers. This allows for making necessary adjustments to accommodate changes in the child’s learning capabilities, as chemo brain may not become apparent immediately.
For most patients, chemobrain improves within 9-12 months after completing chemotherapy, but many people still have symptoms at the six-month mark. A smaller fraction of people (approximately 10-20%) may have long-term effects.
The best way to get a complete picture of your cognitive functioning is to have neuropsychological testing. Your oncologist can refer you for this evaluation. Information from neuropsychological testing can also be extremely helpful to share with your employer or school if you are hoping to get accommodations at work or extra time for exams, homework etc.
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogold #makeseptembergold #childhoodcancer #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
Day 29
Day 29: Relapse
Sometimes, despite the best care and significant progress made in treatment, cancer comes back. When this happens it is called a recurrence or relapse. The likely relapse occurs is that a few of the original cancer cells survived the initial treatment. Sometimes, this is because cancer cells spread to other parts of the body and were too small to be detected during the follow-up immediately after treatment.
The aim of cancer treatment is to remove or destroy all the cancer cells and to reduce the risk of it coming back. However, after treatment, cancer cells can sometimes stay in the body and over time may start to divide and grow again to form a cancer. This can happen very quickly or for some children take years.
Close surveillance is performed on all children, teens and young adults after the end of treatment to check for a recurrence of their cancer. These checks can vary from blood tests to CT scans, x-rays to MRIs. Many children are checked 3 monthly for several years after the end of treatment with the checks becoming less frequent over time.
Every time these checks are done family anxiety levels rise dramatically and the fear of relapse grows. If relapse occurs it is often possible to treat the cancer again and for some children the aim is to get rid of the cancer again. However for other children the aim is to control the cancer, sometimes for many months or years.
Parents and the whole family need ongoing support from friends and family after treatment finishes because the fear of recurrence never truly goes away.
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogold #makeseptembergold #childhoodcancer #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
Sometimes, despite the best care and significant progress made in treatment, cancer comes back. When this happens it is called a recurrence or relapse. The likely relapse occurs is that a few of the original cancer cells survived the initial treatment. Sometimes, this is because cancer cells spread to other parts of the body and were too small to be detected during the follow-up immediately after treatment.
The aim of cancer treatment is to remove or destroy all the cancer cells and to reduce the risk of it coming back. However, after treatment, cancer cells can sometimes stay in the body and over time may start to divide and grow again to form a cancer. This can happen very quickly or for some children take years.
Close surveillance is performed on all children, teens and young adults after the end of treatment to check for a recurrence of their cancer. These checks can vary from blood tests to CT scans, x-rays to MRIs. Many children are checked 3 monthly for several years after the end of treatment with the checks becoming less frequent over time.
Every time these checks are done family anxiety levels rise dramatically and the fear of relapse grows. If relapse occurs it is often possible to treat the cancer again and for some children the aim is to get rid of the cancer again. However for other children the aim is to control the cancer, sometimes for many months or years.
Parents and the whole family need ongoing support from friends and family after treatment finishes because the fear of recurrence never truly goes away.
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogold #makeseptembergold #childhoodcancer #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #childhoodcancerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
Day 30
Day 30: Remission
REMISSION is a word we all want to hear in the cancer world as it means the treatment has worked or helped, at least, even if for only a short time.
Some doctors NEVER use the word CURED as there are simply no guarantees as even after treatment ends there can still be microscopic cells left behind.
A remission is when cancer cannot be detected in the body and there are no symptoms. This may also be called having “no evidence of disease” or NED.
There is often confusion between the terms "cure" and "remission," but it's important to understand that they don't mean the same thing. Cure means that there are no traces of cancer left after treatment and will never come back, while remission means that signs and symptoms of cancer are partially or entirely gone.
There are two types of remissions:
Partial remission: The cancer is still detectable, but there was a reduction of at least 50% in a tumor's size (with solid tumor cancers). In cases of blood cancer, it means fewer cancer cells are circulating in the body. At this stage, doctors will often say that the disease is controlled
Complete remission: Tests, scans, and exams are unable to detect traces of cancer in the body. Doctors also describe it as no evidence of disease (NED). However, some cancer cells may still be present but are undetected by tests
Cancers that return usually do so within the first 5 years, however, they can still come back years later.
Kids in remission are likely to feel better, eat better, and have more energy. Emotionally, kids and their families feel more relaxed and begin to enjoy life more.
Time does help the anxiety of a relapse, however it never truly goes away. The fear never goes away.
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogold #makeseptembergold #childhoodcancer #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #cancermomncerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
REMISSION is a word we all want to hear in the cancer world as it means the treatment has worked or helped, at least, even if for only a short time.
Some doctors NEVER use the word CURED as there are simply no guarantees as even after treatment ends there can still be microscopic cells left behind.
A remission is when cancer cannot be detected in the body and there are no symptoms. This may also be called having “no evidence of disease” or NED.
There is often confusion between the terms "cure" and "remission," but it's important to understand that they don't mean the same thing. Cure means that there are no traces of cancer left after treatment and will never come back, while remission means that signs and symptoms of cancer are partially or entirely gone.
There are two types of remissions:
Partial remission: The cancer is still detectable, but there was a reduction of at least 50% in a tumor's size (with solid tumor cancers). In cases of blood cancer, it means fewer cancer cells are circulating in the body. At this stage, doctors will often say that the disease is controlled
Complete remission: Tests, scans, and exams are unable to detect traces of cancer in the body. Doctors also describe it as no evidence of disease (NED). However, some cancer cells may still be present but are undetected by tests
Cancers that return usually do so within the first 5 years, however, they can still come back years later.
Kids in remission are likely to feel better, eat better, and have more energy. Emotionally, kids and their families feel more relaxed and begin to enjoy life more.
Time does help the anxiety of a relapse, however it never truly goes away. The fear never goes away.
#ccam2022 #childhoodcancerawareness #journeyofaleukemiawarrior #childhoodcancerwarrior #morethan4 #gogold #makeseptembergold #childhoodcancer #childhoodcancerawarenessmonth #ccam #gogoldforchildhoodcancer #gogoldinseptember #leukemiawarrior #lukasstrong #warriorlukas #cancermomncerwarriors #pediatriccancer #pediatriccancerawareness #acutelymphoblasticleukemia #ALL #bloodcancer #leukemia #leukemiaawareness #neverstopfighting #thankfulgratefulblessed #beboldgogold #cancermom
Extra (before September)
Why is it so important to go gold in September?
The simple answer is, “Because it has to begin somewhere” and it all begins with awareness.
The fact that childhood cancer; our nation’s number one killer of children by disease receives so little funding and research is unacceptable and it needs to change. Change will only occur if more people are aware.
If we can color our country gold in September, awareness will grow exponentially, leading to greater funding and research that will save children’s lives and lead to more humane treatments for our kids.
It works! If you don’t believe it does, look what the color pink has done for breast cancer; higher survival rates, earlier detection, and many more drugs developed by the pharmaceutical companies.
Our kids deserve the same.
Please do all you can to help us color the country gold in September.
Please do everything and anything to help make September as gold as October is pink!
It all begins with awareness.
#CCAM #pediatriccancerawareness #childhoodcancer #journeyofaleukemiawarrior #childhoodcancerwarrior
The simple answer is, “Because it has to begin somewhere” and it all begins with awareness.
The fact that childhood cancer; our nation’s number one killer of children by disease receives so little funding and research is unacceptable and it needs to change. Change will only occur if more people are aware.
If we can color our country gold in September, awareness will grow exponentially, leading to greater funding and research that will save children’s lives and lead to more humane treatments for our kids.
It works! If you don’t believe it does, look what the color pink has done for breast cancer; higher survival rates, earlier detection, and many more drugs developed by the pharmaceutical companies.
Our kids deserve the same.
Please do all you can to help us color the country gold in September.
Please do everything and anything to help make September as gold as October is pink!
It all begins with awareness.
#CCAM #pediatriccancerawareness #childhoodcancer #journeyofaleukemiawarrior #childhoodcancerwarrior